Lumbar Disc Herniation: Causes, Symptoms, and Treatment Options
Chronic back pain often stems from issues within the spine’s cushioning system. The term Lumbar Disc Herniation (Lower Back Disc) refers to one of the most common spinal disorders, impacting millions of individuals annually and serving as a leading cause of radiating pain into the leg, known as sciatica. While the pain caused by a herniated Disc can be debilitating, it is crucial to understand that most patients experience significant improvement through non-surgical management alone, typically within four to six weeks. Understanding the underlying structure of the spine, the primary causes of damage, and the comprehensive range of lumbar disc herniation treatment options available is the first critical step toward finding effective relief.
What Is a Lumbar Disc Herniation?
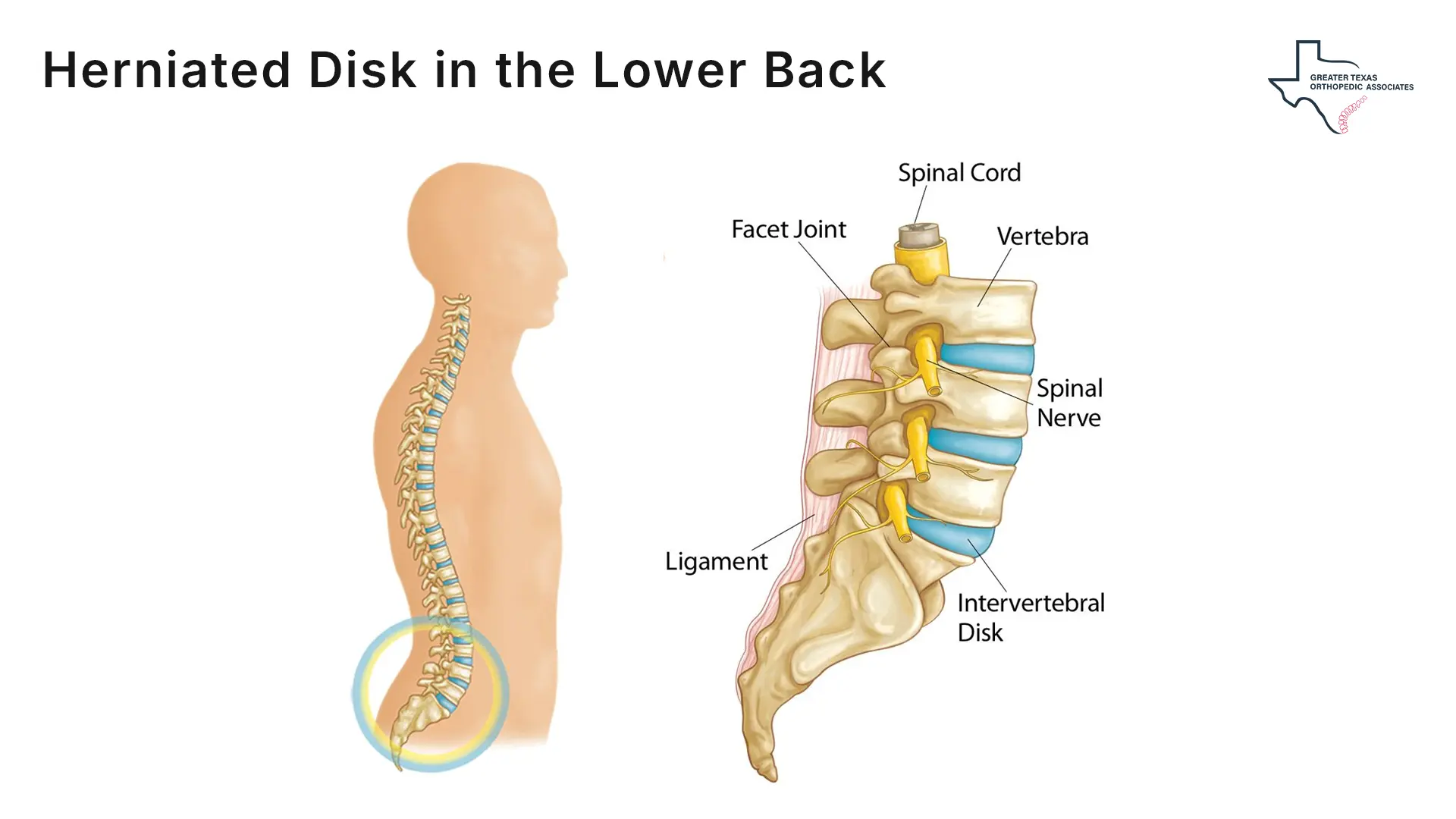
A lumbar disc issue is a structural problem involving the cushions situated between the bones (vertebrae) of the spine. Although herniation can occur anywhere along the spine, it is most prevalent in the lower back, defining a Lumbar Disc Herniation (Lower Back Disc).
Basic Anatomy of the Disc
The human spine is a column of 24 stacked bones (vertebrae) separated by round, flexible intervertebral Discs that act as crucial shock absorbers, enabling mobility and handling physical loads.
Each spinal Disc has a two part composition:
- Nucleus Pulposus (NP): The soft, jellylike center.
- Annulus Fibrosus (AF): The tougher, flexible exterior ring that encases the nucleus.
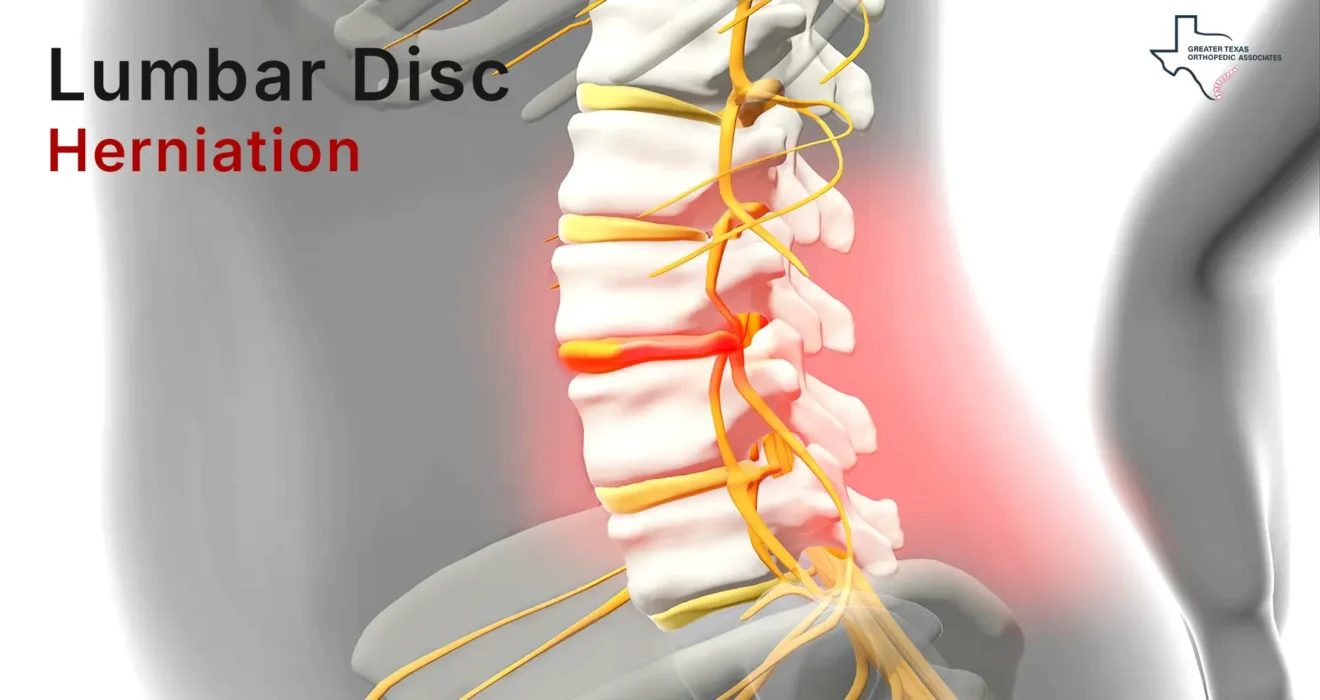
Mechanism of Herniation
A lumbar disc issue occurs when the inner nucleus pulposus pushes out through a tear or crack in the outer annulus fibrosus, placing pressure on the spinal cord or nearby nerve roots.
The compressed nerves are affected by both mechanical pressure and chemical irritation from inflammatory substances released by the disc material. Together, these factors produce pain, numbness, weakness, and other symptoms of nerve root irritation (radiculopathy).
Causes of Lower Back Disc Problems
A single traumatic event rarely causes a herniated lumbar disc; rather, it is most often the result of gradual, cumulative damage and age-related wear and tear.
Age and Degeneration
The most common causes of Lower Back Disc issues involve natural disc degeneration. With age, discs lose water and flexibility, making them prone to small tears or ruptures even with minor strain. Herniated discs occur most often between the ages of 30–50.
Biomechanical Stress and Lifestyle Factors
Several physical and lifestyle factors accelerate Disc vulnerability, contributing significantly to the causes of Lower Back Disc problems:
Improper Lifting: Using the back muscles to lift heavy objects instead of bending the knees and engaging the stronger leg and thigh muscles places extreme strain on the lumbar spine. Twisting and turning while lifting further increases the risk of rupture.
Weight: Excess body weight, particularly around the abdomen, increases pressure on the spinal Discs, making them more susceptible to herniation.
Smoking: Smoking is believed to lessen the oxygen supply to the intervertebral Discs, which accelerates degeneration and makes the Discs vulnerable to damage.
Sedentary Habits: Sitting for long periods, combined with the vibration experienced during frequent driving, can put pressure on the spine. A lack of regular exercise is also a known risk factor.
Lower Back Disc Symptoms
The clinical presentation of LDH varies significantly depending on the location of the herniation and the nerve root being compressed. Since most herniations occur in the lumbar region, the primary symptoms typically affect the lower body.
Common Pain and Nerve Patterns
- Sciatica: Sciatica is characterized by a sharp, shooting, or burning pain that starts in the lower back or buttocks and radiates down one leg, often reaching the calf or foot.
- Numbness or Tingling (Paresthesia): Patients commonly experience a “pins-and-needles” sensation, numbness, or tingling in the parts of the leg or foot served by the affected nerve.
- Weakness: Compression of a nerve can lead to muscle weakness in the leg or foot, sometimes causing foot drop or stumbling.
It is possible to have a lumbar disc issue and experience no symptoms at all, which is known as asymptomatic Disc herniation. Conversely, the first symptom of a herniated Disc is often low back pain, which may subside after a few days, only to be followed by radiating symptoms.
Red Flags Requiring Immediate Care
In rare cases, severe nerve-root compression can cause Cauda Equina Syndrome, a medical emergency that can lead to permanent weakness or paralysis. Seek urgent care if you experience severe Lower Back Disc symptoms:
- Loss of Bladder or Bowel Control: New or worsening incontinence or difficulty urinating.
- Saddle Anesthesia: A progressive loss of sensation in the areas that would touch a saddle (inner thighs, back of legs, and area around the rectum).
- Worsening Weakness: Rapidly increasing pain, numbness, or weakness that severely hampers daily activities or the ability to stand or walk.
Diagnosis
The diagnostic process begins with a thorough clinical examination followed by targeted imaging tests, if necessary, to confirm the diagnosis and rule out other causes of pain.
Clinical Examination
A healthcare provider will assess your medical history, reflexes, muscle strength, and sensation. A common specialized test used to indicate the presence of a herniated Disc is the Straight Leg Raise (SLR) test. During this test, the doctor lifts the affected leg straight up while the patient lies flat on their back; if this causes shooting pain below the knee, it is a strong indication of a Disc herniation.
Imaging Tests
Imaging helps confirm a herniated Disc and visualize affected nerves.
Magnetic Resonance Imaging (MRI) Scan: The most accurate and common test for detecting a herniated Disc.
X-rays: Cannot show soft Discs but rule out fractures, tumors, or spinal misalignment.
Computed Tomography (CT) Scan: Uses cross-sectional X-rays to view the spinal column.
Electromyogram (EMG) and Nerve Conduction Studies: Assess nerve function and muscle activity to identify the affected nerve root.
Treatment Options
The primary goal of lumbar disc herniation treatment is to reduce pain and inflammation while supporting the body’s natural healing. Most patients improve within four to six weeks through conservative, non-surgical approaches, such as rest, medications, and physical therapy. Studies show that up to 76.6% of patients experience spontaneous resorption under these methods, making non-surgical treatment the preferred first-line approach.
At Greater Texas Orthopedic Associates (GTOA), our multidisciplinary team of orthopedic specialists, neurosurgeons, and pain management experts provides comprehensive care, starting with the least invasive options.
Non-Surgical Treatment for Lumbar Herniated Disc
1. Rest, Activity Modification, and Medication
Activity Adjustment: While short periods of rest (one to three days) may be needed for severe pain, prolonged bed rest should be avoided as it can cause muscle stiffness and worsen symptoms. Patients are advised to modify activities, avoiding movements that aggravate pain, such as bending forward and lifting.
Pharmacological Management: Medications are used to manage inflammation and pain.
- Over-the-Counter (OTC) Drugs: Nonsteroidal Anti-Inflammatory Drugs (NSAIDs), such as ibuprofen or naproxen, are used to reduce both inflammation and pain.
- Prescription Drugs: If OTC medications are insufficient, a provider may prescribe muscle relaxants for painful spasms or oral corticosteroids for a short course (typically 7 to 10 days) to powerfully reduce inflammation. Neuropathic drugs (like gabapentin or pregabalin) may be prescribed to affect nerve impulses and decrease pain.
2. Physical Therapy (PT)
Physical therapy is a core component of non-surgical treatment for this condition, aiming to improve mobility, circulation, and muscle support.
- Core Strengthening: Strengthening the trunk muscles (abdomen and core) stabilizes and supports the spine, thereby taking pressure off the Discs.
- McKenzie Method: This specialized form of Mechanical Diagnosis and Therapy (MDT) uses repeated lumbar movements in specific directions (such as extension) to induce centralization, where pain moves from the limb back toward the spine, leading to better outcomes.
- Manual Techniques: Physical therapists may employ mobilization and manipulation techniques to improve joint flexibility, decrease stiffness, and reduce muscle spasms. Deep tissue massage (DTM) or soft tissue mobilization (STM) can enhance circulation and reduce inflammation.
3. Interventional Pain Management (Injections)
When oral medications and physical therapy fail, targeted spinal injections provide an effective non-surgical treatment for herniated lumbar disc by delivering powerful anti-inflammatory medication directly to the source of pain.
Epidural Steroid Injections (ESIs): This minimally invasive procedure involves injecting a corticosteroid and often a local anesthetic directly into the epidural space surrounding the inflamed spinal nerves. ESIs are a common intervention for conditions like herniated discs, sciatica, and spinal stenosis because they aim to reduce nerve irritation and swelling at the source. Many patients benefit from precise epidural steroid injections, an option GTOA provides with image-guided accuracy.
Selective Nerve Root Blocks (SNRBs): SNRBs involve injecting a local anesthetic and sometimes a corticosteroid near the neural sheath of a specific nerve root as it exits the spine. SNRBs serve two primary purposes: diagnostically, they confirm which specific nerve root is causing the pain; therapeutically, they provide temporary relief by blocking pain signals and reducing inflammation.
📌To better understand how these injections work to reduce swelling and irritation around the compressed nerve, we recommend exploring further resources on the ESI procedure: [What is an epidural steroid injection?]
When Surgery Is Considered
For the majority of patients (9 out of 10), symptoms resolve with non-surgical care. Surgery, as a definitive lumbar disc herniation treatment, is typically reserved for those with severe symptoms that persist despite extensive conservative therapy or when emergency neurological issues arise.
Indications for Surgery
A spine specialist may recommend surgical intervention if conservative treatments have failed to improve debilitating symptoms after a period of approximately six weeks or more. Key indications include:
Intractable Pain: Severe pain that is poorly controlled or persists for six weeks or longer despite comprehensive non-surgical management.
Progressive Neurological Deficits: Increasing muscle weakness, numbness, or difficulty standing or walking.
Cauda Equina Syndrome: This rare, acute emergency requires immediate surgery due to the loss of bladder or bowel function.
Common Surgical Procedures
The goal of surgery is spinal decompression, removing pressure from the affected nerve roots.
Microdiscectomy: The most common procedure for a single lumbar disc. It uses a minimally invasive outpatient approach to remove the fragment pressing on the nerve, with a success rate over 95% for leg-pain relief.
Lumbar Laminectomy: Removal of part or all of the lamina to create space around the nerve roots and access the herniated disc when needed.
Spinal Fusion: A stabilization procedure joining two or more vertebrae, rarely required for an isolated disc herniation.
Artificial Disc Replacement (ADR): A motion-preserving alternative to fusion, replacing the damaged disc with an artificial one.
Minimally invasive variations use smaller incisions, reduce muscle disruption, and typically allow faster recovery, often enabling a return to light activity within a few days.
Prevention & Long-Term Management
Preventing a Lumbar Disc Herniation (Lower Back Disc) and managing long-term spinal health involves maintaining spinal strength and adopting careful habits.
Core Stability and Ergonomics
Exercise and Core Strength: Regular exercise, focusing on strengthening the trunk muscles (core and abdomen), is vital as it stabilizes and supports the spine, reducing pressure on the discs.
Proper Posture and Lifting: Maintain good posture, especially when sitting for long periods, to reduce pressure on the spine. When lifting heavy objects, always bend the knees and keep the back straight, ensuring the legs, not the back, bear the majority of the weight.
Lifestyle Adjustments
Maintain a Healthy Weight: Controlling body weight reduces the excess pressure placed on the Discs in the lower back.
Quit Smoking: Avoiding all tobacco products is crucial, as smoking is believed to accelerate Disc degeneration by limiting oxygen supply.
Conclusion
Lumbar Disc Herniation (Lower Back Disc) is a widespread yet manageable cause of spinal pain, created when displaced disc material compresses sensitive nerve roots. Lower Back Disc symptoms can be intense, radiating pain, numbness, or weakness, but the majority of patients improve through conservative care.
In most cases, non-surgical treatment for a herniated lumbar disc provides the body with the time it needs to heal and naturally reduce inflammation. Surgery remains necessary only for patients with persistent, disabling symptoms or worsening neurological deficits.
Navigating spinal health resembles repairing a damaged bridge: most structures regain strength through strategic reinforcement, while only severe or progressive cases require full reconstruction.





3 Comments
Awesome blog.
I rattling thankful to find this internet site on bing, just what I was looking for : D also bookmarked.
Thank you for your kind words! We’re glad you found the information helpful.