What Causes Back Pain? Symptoms of Different Types of Back Pain
Back pain is astonishingly common; most adults experience it at least once, whether as a brief annoyance or a disabling ache that disrupts daily life. The spine is a tightly coordinated system of muscles, discs, joints, and nerves, and even a small disturbance in any of these structures can trigger significant discomfort. Because these parts work so closely together, pinpointing the exact source of pain isn’t always straightforward. Understanding how this system functions and why it fails is the foundation for effectively managing and relieving back pain.
This article explores the fundamental question: what causes back pain?. We will examine the categories of causes, detail the diverse back pain symptoms, and outline the different ways healthcare providers classify varieties of back pain to determine the most effective treatment pathways.
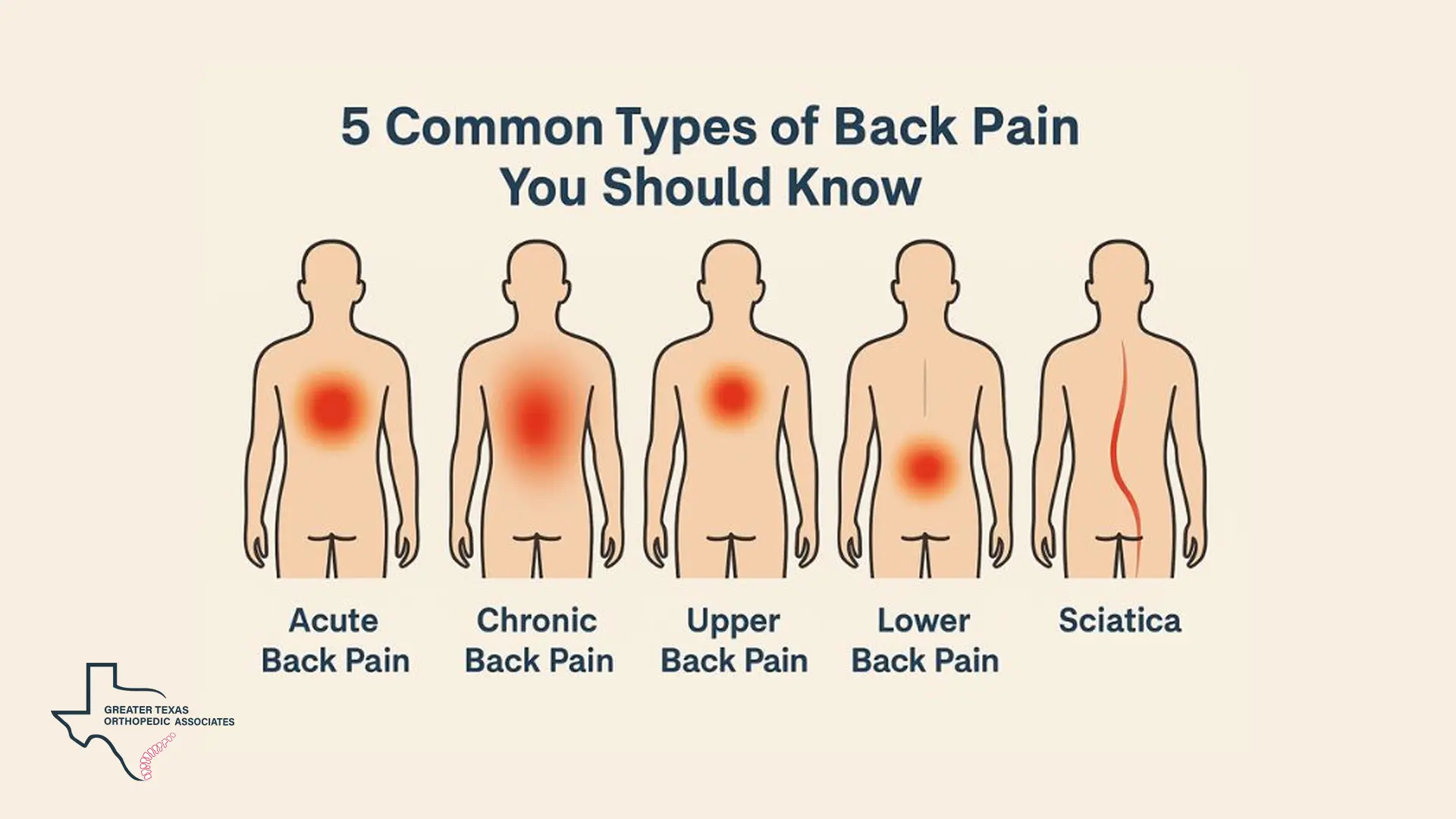
Classifying the Types of Back Pain
Back pain is often classified in two key ways: by duration and by location.
Classification by Duration
The length of time pain persists helps specialists determine the urgency and nature of the underlying issue. The common types of back pain based on duration include:
- Acute Back Pain: Sudden pain lasting less than six weeks, often from injury, usually resolves on its own.
- Subacute Back Pain: Pain that continues for four to twelve weeks, bridging acute and chronic phases.
- Chronic Back Pain: Persistent pain beyond twelve weeks, sometimes from unresolved acute pain or long-term conditions.
Classification by Location
Back pain can occur anywhere from the base of the neck to the top of the buttocks. Healthcare providers often classify pain by the spinal region affected:
- Lower Back Pain (Lumbar Spine): Pain felt below the ribcage in the lumbar region, often occurring because this part of the spine bears most of the body’s weight and is heavily stressed during daily activities like lifting or bending.
- Upper and Middle Back Pain (Thoracic Spine): Pain experienced between the base of the neck and the bottom of the rib cage, which is less common due to the limited flexibility of the thoracic spine, but when it occurs, it can sometimes signal a more serious underlying condition.
Understanding Back Pain Symptoms
The way a patient describes their discomfort, the location of the pain, and any associated sensations are critical clues used for an accurate diagnosis. Common symptoms vary significantly depending on the underlying structure involved.
Descriptive Symptoms
- Muscular Pain: Achy, tight, or spasm-like pain, often worsening with movement, common in strains and sprains.
- Nerve Pain: Sharp, burning, or shooting pain, sometimes accompanied by numbness or tingling.
- Axial Pain: Confined to one spot, often caused by muscle strains or joint issues.
- Referred Pain: Dull and aching, felt in areas away from the source, such as the hips or thighs.
- Radicular Pain (Sciatica): Electric shock-like pain following a nerve path, often with numbness or weakness in the limb.
If you experience back pain symptoms accompanied by severe pain, muscle spasms, loss of bowel or bladder control, or sudden numbness/weakness in your limbs, you should seek immediate care. These are potential signs of serious issues, such as Cauda Equina Syndrome (paralysis of lower spine nerves) or a fracture.
What Causes Back Pain? Exploring the Etiology
Back pain arises from a broad array of conditions across all age groups, though most cases in adults are mechanical in nature or have a nonspecific origin.
Mechanical and Structural Causes
The causes of back pain often stem from direct injury, wear-and-tear, or abnormalities in the spine’s structures:
Strains and Sprains:
Injuries to muscles, tendons, or ligaments from sudden events like lifting, falls, or twisting, or from repetitive stress, often lead to painful spasms.
Disc Pathologies:
- Herniated or Ruptured Discs: When disc material presses on nerves, it can cause intense pain, often resulting in sciatica.
- Degenerative Disc Disease (DDD): Discs weaken over time, causing back pain that may radiate to the limbs and worsen with bending or twisting.
Joint and Bone Issues:
- Arthritis: Chronic inflammation, especially osteoarthritis, can stiffen the spine and cause pain.
- Spinal Stenosis: Narrowing of the spinal canal may lead to lower back pain, sciatica, and leg symptoms, often relieved with rest.
- Fractures: Trauma or osteoporosis can cause vertebral breaks, producing localized pain.
- Spondylolysis and Spondylolisthesis: Vertebral defects or slippage can cause lower back pain and muscle spasms.
- Spinal Curvature (Scoliosis): Severe abnormal curvatures can also lead to discomfort.
These mechanical and structural issues are among the most common factors contributing to back pain, highlighting the complexity of the spine and why accurate diagnosis is crucial.
Systemic and Referred Causes
Back pain can sometimes be a referred symptom, where the source lies elsewhere in the body.
Referred Pain from Organs:
- Kidney Stones/Infection: Pain in the lower back or side, often with fever or painful urination.
- Pancreatitis: Abdominal pain spreading to the back, worse when lying flat.
- Aortic Pathology: Steady, deep pain in the lower back or abdomen, such as from an abdominal aortic aneurysm.
- Gynecological Issues: Conditions like endometriosis or uterine fibroids can cause lower back and pelvic discomfort.
Infections and Tumors:
- Infections: Vertebral osteomyelitis, spinal epidural abscess, or spinal tuberculosis can produce localized, persistent pain, sometimes with fever.
- Tumors: Malignant lesions in spinal structures may cause deep, aching pain that worsens at night or persists at rest.
Inflammatory and Metabolic Conditions:
- Ankylosing Spondylitis: An Inflammatory disease that can fuse spine bones, reducing flexibility and causing back pain.
- Osteoporosis: Weakening of the vertebrae increases the risk of painful compression fractures.
Understanding what causes back pain in these cases is crucial, as they may indicate serious underlying health issues.
Risk Factors and Prevention
Several factors increase an individual’s risk of developing back pain:
- Age: Back pain often begins around age 30 or 40 and becomes more common with age.
- Lack of Exercise/Weak Core: Weak, unused muscles in the back and abdomen (the body’s core) provide poor support for the spine, increasing strain. Regular low-impact aerobic activities, such as walking or swimming, can increase strength and endurance in the back.
- Excess Weight: A body mass index (BMI) greater than 25 puts extra stress on the back muscles and is associated with persistent back pain.
- Smoking: Smoking increases the risk of low back pain and is associated with persistent back pain. This may be due to coughing (leading to herniated discs) and decreased blood flow to the spine.
- Psychological Conditions: People prone to anxiety and depression appear to have a greater risk, and stress can cause muscle tension that contributes to pain.
- Poor Posture: Spending long hours sitting or standing with poor posture can lead to pain over time. This includes slouching or sitting in chairs that lack proper back support.
Preventing recurrence involves patient education and consistent effort. It is important to maintain a healthy weight, avoid smoking, and practice proper body mechanics when lifting. When lifting heavy objects, the legs, not the back, should do the work, keeping the back straight and bending only at the knees.
Diagnosing Back Pain and Recognizing Red Flags
Determining the precise diagnosis for back pain begins with a thorough history and physical examination. The onset, quality, and aggravating/alleviating factors of the pain are carefully considered.
The Diagnostic Process
Our specialists at GTOA use a thorough diagnostic approach to identify the true source of back pain. Our team provides advanced orthopedic care and pain management, ensuring that patients receive an accurate diagnosis and effective treatment.
Evaluation typically includes a detailed assessment of the musculoskeletal and neurological systems, checking range of motion, strength, reflexes, and sensation. When needed, further testing is performed:
Imaging: X-rays for bone issues; MRI for soft tissue and nerve evaluation; CT scans for detailed anatomical imaging.
Specialized Tests: EMG and nerve conduction studies assess nerve function, and image-guided injections such as Medial Branch Blocks help confirm specific pain generators.
When to Seek Immediate Medical Attention
While most back pain is not life-threatening, certain symptoms warrant immediate medical evaluation or a trip to the emergency room:
- New onset of bowel or bladder control problems (incontinence or retention).
- Severe back pain accompanied by fever.
- Pain following a fall, blow to the back, or serious injury, such as a car accident.
- Pain accompanied by numbness, tingling, or weakness in both legs, or saddle anesthesia (numbness around the buttocks or genitals).
- Unexplained weight loss.
If you notice your pain is worse at night or does not improve with rest, this could signal a systemic problem like an infection or tumor, requiring prompt evaluation.
Treatment Approaches for Different Kinds of Back Pain
Treatment for back pain depends heavily on the root causes of back pain and the severity of the symptoms. Many cases have an unidentifiable cause (nonspecific pain).
Conservative Management
For acute, nonspecific back pain without red flags, the first-line treatments are nonpharmacological:
Activity and Rest: Early return to normal routines is recommended, avoiding only heavy labor and activities that precipitate pain. Avoiding long periods of bed rest is crucial. Gentle movement and exercise, such as walking, swimming, or specific stretching/strengthening exercises, can help ease pain.
Temperature Therapy: Superficial application of heat can relieve stiffness or muscle spasms, while ice packs can reduce pain and swelling.
Medication: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are often advised. Muscle relaxants may be used. For chronic low-back pain, exercise therapy and cognitive behavioral therapy (CBT) are considered first-line treatments.
Interventional Pain Management
When conservative measures fall short, minimally invasive procedures help target specific generators of back pain.
Epidural Steroid Injections (ESI):
Deliver corticosteroid medication into the epidural space to reduce nerve inflammation. Commonly used for sciatica, spinal stenosis, and herniated discs, providing temporary but effective relief.
Facet Joint Interventions:
Used when pain originates from the facet joints.
Medial Branch Blocks (MBB): Inject anesthetic near the medial branch nerves to confirm facet joint pain.
Facet Joint Injections (FJI): Deliver anti-inflammatory medication directly into the facet joint for therapeutic relief.
Radiofrequency Ablation (RFA): Performed after successful diagnostic blocks to disrupt pain-signaling nerves and provide long-lasting relief.
📌 For readers who want a deeper breakdown of how MBBs and FJIs compare in treating different kinds of back pain, our article “Medial Branch Blocks vs. Facet Joint Injections: What’s the Difference?” offers a clear, detailed comparison.
Surgical Options
Surgery is generally considered a last resort after conservative and interventional approaches have been exhausted. It is reserved for severe symptoms, failure of non-surgical treatment, or when red flag symptoms (like progressive motor loss or Cauda Equina Syndrome) warrant immediate intervention.
Common Procedures: Surgical techniques include microdiscectomy (for a herniated disc), spinal fusion (joining vertebrae to stabilize the spine), and laminectomy (to treat spinal stenosis).
Minimally Invasive Spine Surgery (MISS): Techniques utilizing smaller incisions and specialized instruments aim to reduce recovery time and muscle damage.
Conclusion: Finding Relief
Back pain is a highly complex and pervasive symptom that necessitates a comprehensive and individualized approach to diagnosis and treatment. Whether the pain is acute (less than six weeks) or chronic (over 12 weeks), identifying the precise causes of back pain is essential for determining the most effective path to recovery.
The vast majority of back pain cases, particularly those caused by muscle strain or sprain, are self-limited and improve with conservative measures such as remaining active and applying heat or ice. However, for those suffering from chronic discomfort, understanding what causes back pain. often involves investigating structural issues like herniated discs, spinal stenosis, or facet joint arthritis.
Specialized types of back pain, such as radicular pain (sciatica) involving nerve compression, require targeted interventions like Epidural Steroid Injections or Radiofrequency Ablation to manage inflammation and interrupt pain signals. Continuous monitoring, adherence to rehabilitation programs (like physical therapy focused on core strengthening), and lifestyle modifications are crucial for both preventing recurrence and ensuring long-term functional recovery.
Ultimately, the key to effectively managing back pain lies in understanding the underlying mechanisms and taking an active role in your care. By focusing on accurate assessment and informed decision-making, patients can address the root causes, improve their function, and achieve long-term relief from the conditions that cause back pain.