Imagine living with chronic back pain that just won’t quit. You’ve tried rest, medication, and therapy, yet the pain persists. Medial Branch Block might be the solution you’ve been searching for. In this article, we cover all about Medial Branch Block. from what it is and how a medial branch block works to its benefits, procedure, and common questions. You’ll learn why doctors use this injection for diagnosing spine pain and how it can offer relief. Let’s dive into this complete introduction and guide, and put you on the path to understanding this pain-relieving procedure.
What Is a Medial Branch Block?
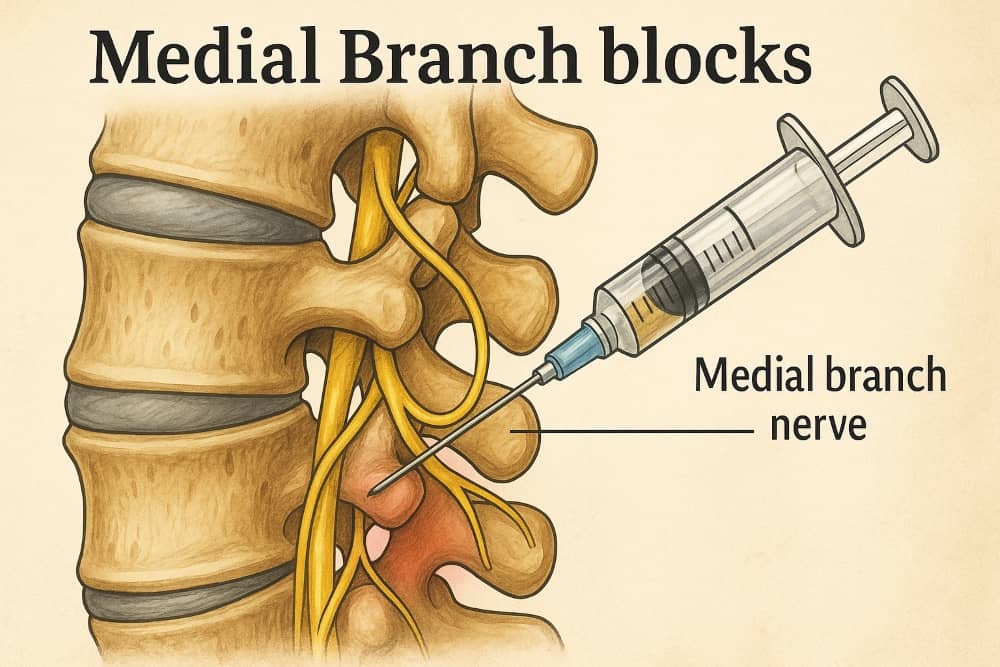
A Medial Branch Block (MBB) is a minimally invasive injection procedure used to block pain signals from the facet joints in the spine. Facet joints are small connections between the vertebrae that contain tiny medial branch nerves, which are responsible for relaying pain signals to the brain. During a medial branch block, the physician administers a local anesthetic, sometimes combined with a steroid, close to the medial branch nerves. This blocks these nerves temporarily, stopping them from sending pain signals from the facet joints to the brain. In simple terms, it’s like putting the phone on mute, the nerves can’t “call” the brain to say the joint is hurting.
Practical Application: Medial branch blocks are most commonly utilized to help diagnose the exact source of spinal pain. If your back or neck pain is suspected to come from arthritis or irritation in the facet joints, an MBB can confirm it by seeing if numbing those nerves relieves the pain. It’s a bit like an investigation. find the pain’s source by numbing specific nerves and observing the result. In some cases, medial branch blocks also provide short-term pain relief, giving patients a break from discomfort while planning the next steps in treatment.
Everyday Example: Let’s say you have persistent lower back pain. Your doctor thinks the pain might be originating from the facet joints (perhaps due to arthritis or facet joint syndrome). They perform a medial branch block by injecting numbing medicine around the small nerve branches serving those joints. If your pain significantly decreases afterward, it tells the doctor that those facet joints were likely the culprit. This not only gives you temporary relief but also guides what to do next for longer-term relief.
Why Is a Medial Branch Block Important?
Identifying Pain Origins:
A key advantage of medial branch blocks is their ability to precisely determine the source of spinal pain, which is important given the many potential causes of back and neck discomfort. This block helps confirm if facet joint problems are to blame. If you experience substantial pain relief, usually defined as at least 80% reduction in pain within the first few hours after the injection, it strongly indicates that the targeted facet joints are the primary source of your discomfort. On the other hand, if there’s no relief, your pain might be coming from another issue, and your doctor will look for other causes. This diagnostic clarity prevents unnecessary treatments and focuses therapy on the right problem.
Planning Further Treatment:
Medial branch blocks are often a precursor to a more long-lasting solution called radiofrequency ablation (RFA). RFA (also known as radiofrequency rhizotomy) uses heat to deactivate the same medial branch nerves, providing pain relief for 6-12 months or more by stopping the nerve from sending pain signals. However, RFA is only effective if we’ve correctly identified the painful joint. That’s why a successful medial branch block (meaning you had good pain relief from it) is usually required before proceeding to RFA. In essence, the block acts as a test run – if numbing the nerve helps, then “shutting it off” with RFA has a high chance of helping too.
Avoiding Unnecessary Procedures:
By confirming the pain source, medial branch blocks can save patients from more invasive treatments or surgeries that might not address the real issue. For example, rather than jumping into spine surgery, a doctor might use MBB to ensure the pain isn’t from facet joints first. If it is, then a less invasive RFA can be done instead of surgery. This targeted approach is safer, often effective, and part of why pain specialists value MBBs.
Therapeutic Relief:
While diagnosis is the main goal, medial branch blocks can also provide therapeutic benefits. The prompt pain relief provided by the local anesthetic may last anywhere from several hours up to a few days. In some cases, especially if a corticosteroid is included, patients might enjoy relief for several weeks or a couple of months as the steroid reduces inflammation around the facet joint nerves. This isn’t permanent, but it can improve quality of life in the short term. It’s worth noting that regular facet joint injections (directly into the joint) or epidural injections are other options for therapeutic relief; the medial branch block primarily shines as a diagnostic test, with any pain relief being a very welcome bonus.
When and Who Should Consider a Medial Branch Block?
Ideal Candidates:
If you have chronic neck or back pain and your doctor suspects it’s coming from arthritis or irritation in your facet joints, you might be a candidate for a medial branch block. Common conditions that cause facet joint pain include facet joint osteoarthritis (spondylosis), degenerative disk disease with facet stress, degenerative spondylolisthesis, or injuries causing facet inflammation. Patients often report pain that is worse with twisting or arching the back, which are movements that stress the facet joints. If other treatments (like anti-inflammatory medications and physical therapy) haven’t fully helped after a few months, a doctor may suggest an MBB to further evaluate the pain.
Diagnostic Use:
For someone who might need an RFA, the medial branch block is an important step. It’s usually considered after more conservative treatments have been tried. Doctors use it to confirm that the facet joints are causing pain before doing the nerve ablation. For example, a patient with facet arthritis who still has pain after physical therapy might get a medial branch block. If it works well, they can move on to RFA for longer relief. If it doesn’t, it saves them from an unnecessary procedure and prompts the doctor to look for other pain sources.
Therapeutic Use:
In some scenarios, medial branch blocks are done for short-term pain relief, even if no further procedure is planned. For instance, if a patient cannot undergo RFA due to other health reasons, periodic medial branch blocks with a small dose of steroid might be used to manage pain intermittently. However, there is a limit to how often steroid injections can be given safely. Generally, if facet joint pain is confirmed, RFA is preferred for longer-lasting relief without the side effects of repeated steroids.
Who Performs It:
A medial branch block is typically performed by a pain management specialist, anesthesiologist, or physiatrist (rehabilitation doctor) with expertise in interventional spine procedures. Orthopedic spine specialists or neurologists trained in pain procedures can also perform it. It’s done in a clinic or outpatient setting, not requiring full surgery.
Patient Preparation:
Doctors will assess if you’re a good candidate. There are some contraindications and precautions. For example, if you’re on blood-thinning medication (like warfarin) or have an active infection or uncontrolled diabetes, the procedure might be delayed or done with special precautions. It’s important to inform your doctor of all your medications and allergies. They’ll likely ask that you arrange a ride home after the injection, since you shouldn’t drive immediately afterward (both because of possible numbness and, if sedation is used, you’ll be groggy).
How a Medial Branch Block Is Done (Step-by-Step)
When you arrive for a medial branch block appointment, knowing what to expect can ease any anxiety. Here’s a step-by-step guide through the procedure:
Step 1: Preparation and Positioning
You’ll be asked to lie down on an X-ray table, usually on your stomach (prone position). The area of your back or neck where the injection will occur is cleaned thoroughly with antiseptic. In many cases, you’ll remain fully awake. Some clinics offer a mild sedative or an IV relaxant, especially if you’re very anxious, but often only a local anesthetic is used to numb the skin at the injection site. The feeling is a quick sting or burn for a few seconds when the numbing medicine is injected into the skin. after that, the area becomes numb.
The medical team will use imaging guidance to perform the block. Typically, fluoroscopy (a type of real-time X-ray) is used to visualize your spine and guide needle placement. In some cases, they might use a CT scan or ultrasound, but fluoroscopic guidance is most common for spine injections. A contrast dye is usually injected at the start to verify that the needle is correctly placed near the medial branch nerve and not inside a blood vessel. This imaging step helps ensure both the safety and precision of the procedure.
Step 2: Needle Insertion and Injection
Once the skin is numb, the doctor advances a thin needle toward the medial branch nerves. Keep in mind that these nerves travel alongside the facet joints. Thanks to the X-ray guidance, the doctor can navigate the needle to the exact target. You might feel some pressure, but sharp pain is uncommon since the area is numbed. If at any point you do feel sharp pain, you should communicate that to your doctor – it could mean the needle is irritating a nerve and they may adjust its position.
When the needle is confirmed to be in place, a small amount of local anesthetic is injected around the nerve. Often this is lidocaine or bupivacaine (numbing agents). Sometimes a small dose of corticosteroid is added to help reduce inflammation. The injection itself is usually brief. You may feel a sensation of pressure or mild discomfort, but many patients find it quite tolerable and quick. The entire procedure often takes about 20-30 minutes, including the setup and the recovery observation afterward.
During the injection, the medical team might ask if you feel any symptom like tingling or reproduction of your typical pain, this can help confirm the needle’s location. However, often you just feel nothing more than the pressure. Because only a small amount of medication is used, the numbing effect is quite localized to those target nerves.
Step 3: Immediate Aftermath and Observation
After the injection, you’ll be observed for a short time (usually 15-30 minutes) to ensure you don’t have any immediate reaction or complications. The staff will also ask you to start moving in ways that would normally trigger your pain. The goal is to test the effectiveness of the block right away. If you suddenly feel a lot better doing those movements (for example, bending or twisting your back with much less pain), it’s a strong indication the block hit the right spot.
Typically, doctors expect medial branch blocks to produce immediate pain relief if they’re effective, specifically, relief within the first 4-6 hours, because that’s how long the local anesthetic works. You might be given a pain diary or worksheet to record how much relief you experience and for how long (e.g., note the pain level over the next several hours and days). This information is crucial for your doctor. For instance, if you experience at least 80% pain relief in that numb period, it’s considered a positive diagnostic result, meaning the facet joint nerves are likely the source of pain. If you experience little to no relief, the test is negative, and your pain may be stemming from a different structure.
After the brief monitoring, assuming you feel fine, you’ll be discharged the same day. Make sure someone is available to drive you home, especially if you had any sedative. Even without sedation, you may feel a bit sore or your muscles might feel weak or numb temporarily, so it’s not safe to drive. The doctor will advise you to take it easy for the rest of the day. Most people can resume normal light activities by the next day.
Results and Recovery
Interpreting the Results: As mentioned, the hours following the medial branch block are very telling. Here are the typical scenarios you might experience after a block:
Significant Immediate Relief:
Your pain significantly diminishes (for example, an 8/10 pain becomes 1 or 2/10). This relief lasts a few hours while the anesthetic is active. This is a positive result, indicating that the blocked medial branch nerves were carrying the pain. In this case, you will likely be considered for a radiofrequency ablation to provide longer-lasting relief.
Partial or Short-Lived Relief:
Maybe you feel somewhat better, but not dramatic improvement, or pain relief lasts only a day or two. This could still mean the facet joints are involved, but the result is not as clear-cut. Your doctor might repeat the block (sometimes doctors perform two diagnostic blocks to be sure) or consider other diagnostic tests. Some relief might also come from the steroid reducing inflammation, which can take a couple of days to kick in.
No Relief:
If you feel no improvement in your pain in the first 4-6 hours after the block, then the facet joints likely aren’t the main source of your pain. This is a negative result. Your doctor will then focus on other potential causes (such as discs, nerves, or muscle sources) and you’ll pursue different treatments rather than facet joint RFA. It can be disappointing not to get relief, but it’s valuable information because it saves you from undergoing an ineffective procedure. In this scenario, the medial branch block has essentially ruled out the facet joints as the pain generator.
But don’t worry, our specialists are ready to help you recover. If you need orthopedic services and pain management and relief throughout Texas, our experienced specialists at GTOA are ready to provide the best and most professional services for your recovery and health.
Recovery and Activity:
Medial branch blocks are outpatient procedures, and recovery is generally quick. You might have some soreness at the injection site once the numbing wears off, this is normal and usually mild. An ice pack on the area for 20 minutes at a time can help, as can a mild pain reliever like acetaminophen if needed (though your doctor may ask you not to take any pain medicine for the first 4-6 hours after the block so that it doesn’t mask the diagnostic results).
Most people are back to their usual activities by the next day. Just avoid strenuous activities or heavy lifting for about 24 hours after the injection. This gives the injection site time to begin healing and reduces any risk of bleeding. If you received sedation, it’s normal to feel drowsy for several hours afterward, so it’s best to take it easy and rest for the rest of the day.
Follow-Up: Your healthcare provider will follow up with you (often within a week) to discuss the results. If the block was positive (effective), they will likely schedule you for radiofrequency ablation of the medial branch nerves for longer relief. RFA is typically done a couple of weeks after a successful block, and it can provide many months of pain relief by essentially quieting those nerves for an extended period. If the block wasn’t helpful, the doctor might order imaging (if not already done) or other diagnostic injections to investigate other structures. Either way, the medial branch block guides the next step in your care plan.
Multiple Levels and Repeat Blocks: Sometimes, pain comes from multiple facet joints. Doctors can perform medial branch blocks at multiple levels in one session (for example, numbing nerves at L3, L4, and L5 levels to cover the facet joints from L3-L4, L4-L5, and L5-S1). This is common because if one facet is arthritic, often adjacent ones are too. If the initial block does not provide clear results, a second confirmatory block may be scheduled on another day. However, medial branch blocks are not usually repeated many times purely for pain relief. if one or two diagnostic blocks confirm facet pain, the goal is to move to RFA rather than keep giving numbing injections over and over.
Risks and Safety of Medial Branch Blocks
It’s reassuring to know that medial branch block injections are typically safe and well-tolerated by the majority of patients. Since this procedure has been performed for decades, doctors have a good handle on its safety profile. But like any medical intervention, there are some risks and side effects to be aware of:
Common Side Effects
Typical side effects tend to be minor and temporary. They include:
Injection site pain or soreness:
It’s not unusual to have some tenderness or bruising where the needle went in. This typically resolves in a day or two. Applying an ice pack may help alleviate this mild discomfort
Temporary numbness or weakness:
Because the anesthetic can spread to nearby nerves, you might feel numb or weak in your back or an arm/leg for a few hours. For example, a lumbar (lower back) block might cause temporary leg numbness. This sensation typically fades as the effects of the anesthetic diminish.
Vasovagal reaction:
A fancy term for feeling lightheaded or dizzy, maybe even fainting. Some people get nervous with needles or have a drop in blood pressure, the clinic staff is prepared for this and will monitor you. It’s brief and not dangerous in most cases.
Headache or flushing:
If a steroid is used, you might get a brief headache, face flushing, or slight temperature elevation later that day. This is sometimes called a “steroid flush” and fades on its own.
Uncommon Risks:
Serious complications are rare, especially when the procedure is done with proper imaging guidance and sterile technique. However, they can include:
Infection:
Anytime a needle breaks the skin, there’s a small risk of infection. Clinics use strict sterile procedures to minimize this. Infection rates for these injections are very low (often less than 0.1%). If an infection does occur, it can usually be treated with antibiotics.
Bleeding:
The needle could hit a blood vessel, or if you have a bleeding tendency, a hematoma (bruise) could form. This is why you must inform your doctor about blood thinners. Significant bleeding is rare, but if you have a bleeding disorder the procedure might be postponed.
Allergic reaction:
This could be a reaction to the contrast dye (if used) or to the medications injected (like local anesthetic or steroid). It’s uncommon, but if you have many allergies, discuss them with your doctor beforehand. They may use alternative medications if needed.
Nerve injury:
This is extremely rare, but if the needle were to accidentally damage a nerve or the spinal cord, it could cause complications like numbness, weakness, or in very rare instances paralysis. Using X-ray guidance and proper technique makes this highly unlikely. Most doctors have never seen this complication in their career, but it’s listed for completeness.
Increased pain:
Paradoxically, a few patients might feel worse pain after the injection. This could be due to irritation from the needle or steroid (“post-injection flare”). It usually subsides in a day or two, and icing can help. If pain dramatically worsens or you have symptoms like high fever or loss of bladder/bowel control after an injection, seek medical attention right away. those could signal a rare complication needing prompt care.
Long-Term Considerations:
Medial branch blocks themselves don’t cause long-term harm to the nerves, the anesthetic’s effect is temporary. However, if steroids are used repeatedly, there are potential long-term side effects from steroid exposure (like elevated blood sugar, bone thinning, hormonal changes). This is why if multiple injections are needed, doctors space them out and use the lowest effective steroid dose, or they move on to non-steroid treatments like RFA. Fortunately, RFA can reduce the need for repeated steroid use by giving longer relief without medication.
Overall, the safety profile of this procedure is excellent. The rate of complications reported in medical studies is very low. If you live in Texas, our specialists in Arlington, Houston, San Antonio, Dallas, Corpus Christi and Beaumont will take every precaution to ensure that your medial branch block is performed safely, using advanced imaging guidance and strict protocols. If you have concerns about the risks, it’s always okay to ask questions.
FAQs about Medial Branch Blocks
Here we address some common questions patients have about medial branch blocks:
What does a medial branch block do, and how does it work?
A medial branch block temporarily numbs certain medial branch nerves in your spine, interrupting pain signals sent from the facet joints. By injecting a local anesthetic around these nerves, the block prevents pain signals from reaching your brain. If your pain eases significantly after the injection, it indicates that those nerves (and the joints they innervate) are the source of your pain. In short, what it “does” is diagnose facet joint pain – and as a bonus, it can give short-term pain relief by turning off those pain messages for a while.
What is a medial branch block used for?
A medial branch block is used for diagnosing and managing facet joint pain in the neck or back. Doctors use it when they suspect conditions like facet arthritis, spinal osteoarthritis, or other spine issues where facet joints are painful. It helps confirm the diagnosis. Additionally, it’s used to predict success for radiofrequency ablation (RFA). If the block is successful, the patient can be scheduled for RFA, which is used to provide longer-term pain relief by deactivating the medial branch nerves. In some cases, medial branch blocks are also used to provide immediate pain relief or to reduce inflammation (if steroid is included), giving the patient a window of relief that can last days or weeks. However, if pain relief is the primary goal and not just diagnosis, doctors might opt for facet joint injections or RFA directly.
So, in summary, medial branch blocks are used to identify facet joint pain and to guide further treatment, and they can also temporarily alleviate pain in the process.
Is getting a medial branch block painful?
It’s normal to be nervous about any injection, but most patients handle medial branch blocks very well. You will feel a pinch and burn with the local anesthetic at the start – similar to a routine shot at the doctor’s office. After that, the area is numbed. You might sense pressure or a minor ache as the needle is positioned and the medication is injected, but it shouldn’t be sharply painful. The procedure is relatively quick (often 20-30 minutes), and any discomfort typically stops once the needle is removed. If you’re especially anxious, ask your doctor, they may offer a mild sedative to help you relax.
Overall, many people find the anticipation is worse than the actual injection. The relief afterward, especially if it takes away your usual pain, often makes it well worth it.
How long does pain relief from a medial branch block last?
The pain relief provided by the numbing medication in a medial branch block is typically short-lived, lasting from just a few hours up to a couple of days as the anesthetic’s effects gradually wear off. If a steroid was injected, you might get an extended relief for a few weeks, since steroids can reduce inflammation around the facet joint nerves. However, some people do not get any pain relief from the block, which indicates it wasn’t the right target for their pain. It’s important to remember the primary goal of a diagnostic block is to see if you get relief at all, rather than to cure the pain.
If you do get good relief, the next step (radiofrequency ablation) can provide a much longer period of relief, often several months of reduced pain. In contrast, if the block doesn’t give you relief, your doctor will pivot to other treatments. In either case, the block’s effect is not permanent, it either sets you up for another procedure or it helps redirect your diagnosis. Consider the medial branch block as a temporary diagnostic tool that can help guide your path toward a more lasting treatment solution.
What are the next steps if the medial branch block is successful?
If your medial branch block significantly relieved your pain (a positive test), congratulations, not only did you get temporary relief, but you and your doctor have likely found the pain generator. The typical next step is to proceed with radiofrequency ablation (RFA) of the medial branch nerves. RFA is performed as an outpatient procedure in which focused heat is applied to cauterize the nerve, blocking its ability to transmit pain signals for a prolonged period, often several months, until the nerve eventually regenerates. Until then, you may enjoy a substantial reduction in pain. In the interim before RFA, your doctor might allow you to have another block if needed, but usually they move forward to scheduling the ablation rather than repeating too many blocks.
If the block is not successful (negative test), the next steps would be different: your doctor might suggest imaging studies (if not already done) like an MRI to look for other pain sources, or try other diagnostic injections (for example, a discogram if a disc issue is suspected, or a different nerve block). The information from a negative block is still useful, it narrows down the list of what’s causing your pain so you don’t undergo unnecessary treatments.
Conclusion
Key Takeaways: Medial branch blocks play an important role in the field of pain management. It’s essentially a diagnostic test that can provide short-term relief and, more importantly, answer the question: “Are my facet joints causing my pain?” By temporarily numbing the tiny nerves to those joints, doctors glean crucial information that guides further treatment. If you’re struggling with chronic back or neck pain from arthritis or facet issues, an MBB might be the stepping stone to longer-lasting relief via radiofrequency ablation. This procedure is quick, low-risk, and often performed right in the clinic.
In summary, medial branch blocks work by blocking pain signals, are used to diagnose facet joint pain, and help tailor the right treatment plan for you. Patients often find the procedure easier than expected and the clarity it provides is invaluable. If you believe your pain may be stemming from facet joints, talk to a pain specialist about whether a medial branch block is appropriate.




6 Comments
Well said, The piece felt detailed and covered everything I needed.
Many thanks. Wonderful َarticle
Great article, i visit this blog often and always find valuable information about orthopedic care and legal medical support in Texas.
Keep up the excellent work
We truly appreciate your continued support.
I’ll be sharing this with my team.
I usually spend some time reading the content on this website along with a cup of coffee. The explanations about medial branch blocks were clear and informative.