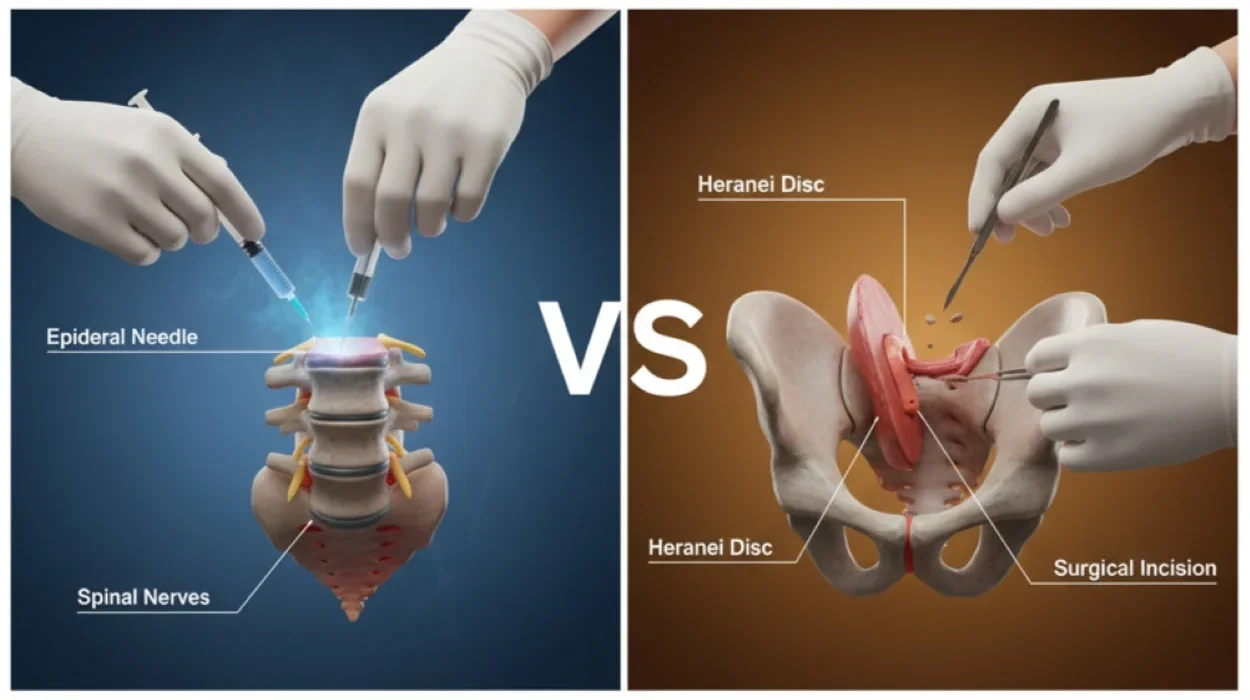
Epidural Steroid Injections vs Surgery for Back Pain: Your Treatment Options
Chronic back pain can be a relentless enemy that disrupts daily life. If you’ve been living with this persistent discomfort for three months or longer, you understand the frustration of seeking effective relief. The journey to a pain-free life often involves exploring various treatment pathways, and two prominent options that frequently come into discussion for back pain in Texas are Epidural Steroid Injections vs Surgery for Back Pain and spinal surgery.
Understanding the benefits and drawbacks of each can empower you to make an informed decision for your spine health. At Greater Texas Orthopedic Associates (GTOA), our experienced team is dedicated to helping patients throughout Texas find lasting relief. We believe in a personalized approach, thoroughly investigating the root cause of your pain and crafting a treatment plan that feels right for you.
Understanding Chronic Back Pain and Its Impact
Chronic back pain is a widespread global issue affecting many adults, leading to disability, lost work productivity, and a substantial socioeconomic burden. Defined as pain lasting three months or longer, it can manifest as localized discomfort from muscle strain or degenerative disc disease, or as radiating pain (lumbar radiculopathy) with numbness, tingling, or weakness, often due to nerve root compression. Pinpointing the exact cause of chronic back pain can be challenging.
Our team at GTOA prioritizes a comprehensive diagnostic approach to identify the pain source for effective treatment. If the cause remains unclear or untreatable, the focus shifts to a pain management plan aimed at reducing pain, improving function, and enhancing overall quality of life.
Initial Conservative Approaches for Back Pain
Before considering interventional procedures or Spinal Surgery, a comprehensive approach to managing Chronic Back Pain often begins with conservative, non-invasive treatments. These foundational steps can significantly improve symptoms and potentially prevent the need for more aggressive interventions.
Diet Change:
Certain diets, particularly those high in trans fats, refined sugars, and processed foods, can be highly inflammatory and may contribute to Chronic Back Pain.
Lifestyle Modifications:
Adapting daily behaviors can play a crucial role. Learning to pace yourself, taking breaks during strenuous activities, and asking for help with heavy objects can minimize strain. Minimizing harmful habits like smoking is also vital, as it can heighten pain and delay healing.
Physical Therapy and Exercise:
Strengthening the muscles around the spine through targeted physical therapy and exercises is a common and effective conservative treatment. This can improve mobility, stability, and overall function, forming a cornerstone of any long-term pain management plan.
These conservative treatments are often the first step in managing persistent pain, offering a low-risk approach with gradual improvements.
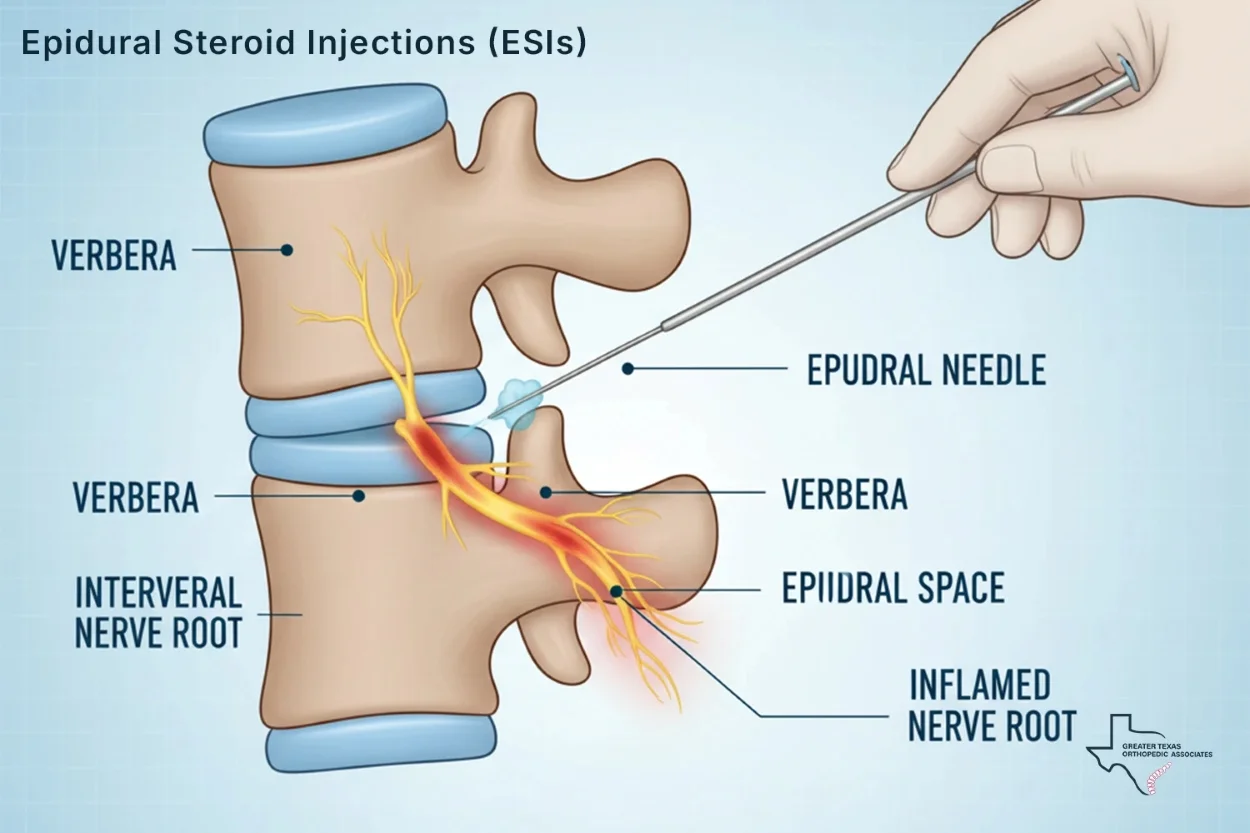
Epidural Steroid Injections (ESIs): A Minimally Invasive Option
Epidural Steroid Injections (ESIs) are a common interventional pain management technique used to alleviate Chronic Back Pain, especially when it radiates into the limbs. These injections are considered a less invasive alternative to Spinal Surgery and are often explored when conservative treatments like physical therapy and medication have not provided sufficient relief.
What Are Epidural Steroid Injections?
An Epidural Steroid Injection (ESI) involves injecting a powerful anti-inflammatory medication, typically a corticosteroid (like cortisol or triamcinolone acetonide) and often a local anesthetic, directly into the epidural space surrounding the spinal nerves. This space acts as a pathway for pain signals from inflamed nerves to the brain. By delivering medication directly to the inflamed nerves, ESIs aim to reduce inflammation and block pain signals, thereby decreasing your pain level. The procedure is performed in an outpatient setting, with patients remaining awake.
📌For a deeper understanding of this procedure, you can explore this article: [What is an epidural steroid injection?].
Conditions That ESIs Can Treat
ESIs are often recommended for specific spinal conditions where nerve inflammation is a primary driver of pain. These include:
- Sciatica
- Herniated Disc
- Spinal Stenosis
- Lumbosacral Radicular Pain
Our team will carefully review your specific case and diagnostic imaging to determine if an ESI is the right choice for you.
The Pros of Epidural Steroid Injections
Minimally Invasive:
ESIs are performed in an outpatient setting and involve a simple injection, avoiding large incisions and general anesthesia associated with surgery.
Rapid Pain Relief:
Studies show ESIs provide short-term (under 1 month) and intermediate-term (1-3 months) pain relief for lumbosacral radicular pain, improving quality of life and enabling participation in other therapies.
Improved Functional Outcomes (Short-term):
Patients who received ESIs reported more successful outcomes compared to those receiving conservative treatment in terms of successful events (defined by pain reduction), particularly in the short-to-intermediate term.
Lower Risk Profile:
Compared to major surgery, ESIs generally carry a lower risk of serious complications.
Cost-Effectiveness for Sciatica:
For sciatica secondary to a herniated lumbar disc, transforaminal epidural steroid injection (TFESI) was found to be less costly as an initial alternative to surgery (microdiscectomy) while achieving similar levels of improved outcomes at 18 weeks.
The Cons of Epidural Steroid Injections
Temporary Relief:
The pain-relieving effects of ESIs are generally temporary, lasting weeks to several months. While some may experience relief for up to a year, repeated injections are often necessary to maintain pain control. However, the effectiveness can diminish over time with repeated injections.
Not a Long-Term Solution for Functional Improvement:
Despite short-term pain relief, ESIs do not show statistically significant advantages over conservative treatment in terms of long-term functional improvement (6 months to 1 year) or even short-to-intermediate term functional improvement (1 to 6 months).
Limited Frequency:
Due to potential side effects of corticosteroids, there are limits on how often ESIs can be administered, typically every few months, and generally not more than twice in a 4-6 week period if relief is not lasting.
Potential Side Effects and Risks:
While generally safe, ESIs can have side effects, including temporary post-injection soreness, dizziness, headaches, and a temporary increase in blood pressure or blood sugar for diabetic patients.
Variable Effectiveness:
The success rate for pain relief can vary, and if an ESI doesn’t work, it indicates the pain source may be something other than nerve inflammation, requiring further investigation.
Exploring Other Interventional Pain Management Techniques
Beyond ESIs, GTOA offers a range of other minimally invasive interventional therapies that might be suitable for your chronic back pain, especially if it originates from the facet joints.
These procedures are often considered as stepping stones to more definitive treatments or as standalone solutions for managing pain.
Medial Branch Blocks (MBBs)
Medial branch blocks are primarily diagnostic tools used to pinpoint if pain originates from the facet joints of the spine. These injections target the medial branch nerves that transmit pain signals from the facet joints. If an MBB provides significant, albeit temporary, relief, it indicates that the facet joints are likely the source of your pain, guiding further treatment options like radiofrequency ablation or physical therapy. A positive block is generally considered when there is at least 50% relief of pain for the expected duration of the local anesthetic.
📌Learn more about this diagnostic technique in this article: [Medial Branch Blocks: Uses, Procedure, Benefits, and FAQs].
Facet Joint Injections (FJIs)
Facet joint injections deliver local anesthetic and/or corticosteroids directly into the facet joint capsule. Like MBBs, FJIs can serve both diagnostic and therapeutic purposes, helping to confirm facet joint pain and provide relief by reducing inflammation within the joint. Studies suggest that FJIs may offer immediate pain relief with potentially fewer complications and higher patient satisfaction compared to MBBs. This may be due to the localized anti-inflammatory effects of corticosteroids and improved joint mobility.
📌For a comprehensive guide, read our article: [All About the Facet Joint Injections Procedure].
Radiofrequency Ablation (RFA)
If a diagnostic medial branch block or facet joint injection successfully relieves your pain, our team may recommend radiofrequency ablation. RFA is a procedure that uses heat generated by radio waves to create a lesion on the nerve, interrupting its ability to transmit pain signals. This can provide longer-lasting relief, often for several months or even years, by effectively “shutting off” the pain signals from the targeted nerves. The most rigorous patient selection for RFA, involving dual medial branch blocks with 100% pain relief and parallel electrode placement, can lead to 56% of patients experiencing complete pain relief at six months.
📌Discover more about this advanced pain relief option: [What is Radiofrequency Ablation (RFA) and What Is…].
These interventional treatments, offered by our pain management specialists at GTOA, represent a crucial step in managing chronic back pain without immediately resorting to spinal surgery.
Considering Surgical Options for Back Pain
When non-surgical treatments, including repeated injections, no longer provide adequate relief, or if your condition presents “red flag” symptoms, spinal surgery may become a necessary and highly effective consideration. Surgery is generally considered a last resort after more conservative options have been exhausted.
When Is Surgery a Good Idea?
Spinal surgery might be recommended for chronic back pain if a clear cause is confirmed by imaging, and other treatments have failed to provide sufficient relief. Additionally, certain “red flag” symptoms warrant immediate surgical evaluation if they are related to your spine condition:
- New or worsening bowel/bladder issues (incontinence, groin numbness).
- Weakness in limbs.
- Gait and balance problems.
- Evidence of increased (brisk) reflexes.
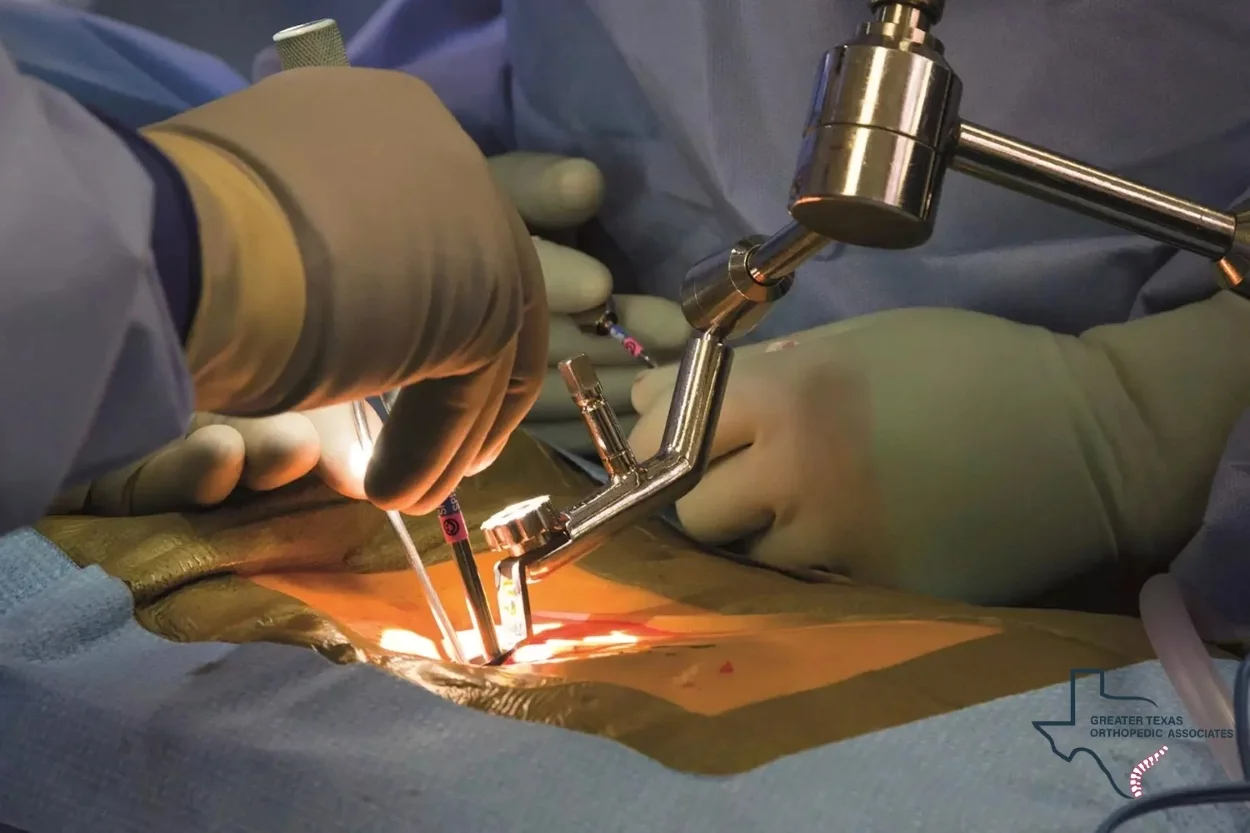
Types of Spinal Surgery
Modern spinal surgery encompasses various techniques tailored to address specific conditions:
Microdiscectomy:
This minimally invasive procedure is often used for herniated discs causing sciatica, where the damaged portion of the disc compressing a nerve is removed.
Spinal Fusion:
This procedure joins two or more vertebrae, often using bone grafts, to stabilize the spine, correct deformities, and relieve nerve compression. It is commonly used for conditions like degenerative disc disease, spondylolisthesis, and when decompression surgery can lead to instability.
Minimally Invasive Spine Surgery (MISS):
Utilizing smaller incisions, specialized instruments, and advanced imaging (like lasers and endoscopic cameras), MISS aims to reduce muscle damage, lessen post-operative pain, and facilitate a quicker recovery, with patients often returning to daily activities within weeks.
Cervical Disc Replacement (CDR):
An excellent alternative to cervical fusion, CDR alleviates nerve pressure while preserving spinal mobility and is clinically proven to reduce the chance of needing further surgery at adjacent levels.
The Pros of Spinal Surgery
Targeted Treatment of Root Cause:
Unlike injections that primarily manage symptoms, surgery can directly correct structural abnormalities contributing to back pain, such as a herniated disc or spinal stenosis.
Potentially Permanent Relief:
For many patients, especially those with severe, debilitating pain unresponsive to other treatments, surgery can provide long-term or permanent relief from chronic back pain, dramatically improving mobility, function, and overall quality of life.
Advanced Techniques:
Significant advancements in surgical techniques, including minimally invasive and robotic-assisted methods, mean smaller incisions, less tissue disruption, reduced blood loss, and potentially faster recovery times.
Correction of Instability and Deformity:
For conditions where decompression causes instability, or in cases of severe spinal deformity, fusion surgery can effectively stabilize the spine.
The Cons of Spinal Surgery
Invasive and Irreversible:
Surgery is the most invasive treatment option and is an irreversible procedure.
No Guarantee of Pain Relief:
While often highly effective, surgery does not guarantee complete pain relief and may, in rare cases, even worsen the pain.
Significant Risks and Complications:
All surgical procedures carry risks. Spinal surgery risks can include nerve injury, infection, bleeding, or a dural tear.
Prolonged Hospitalization and Recovery:
While minimally invasive techniques reduce recovery time, it is generally longer than for injections.
Adjacent Segment Disease (for fusions):
A fused segment may cause increased stress on the levels directly above and below it, potentially leading to degeneration in those areas over time.
Questionable Long-Term Efficacy for Chronic Low Back Pain:
A meta-analysis comparing surgical fusion to non-surgical intervention for chronic low back pain found only a marginal, non-statistically significant improvement in the Oswestry Disability Index (ODI) in favor of surgery. This difference was considered “minimal clinical importance,” and the study concluded that current evidence does not support routine surgical fusion for chronic low back pain, recommending caution from surgeons.
Your Path to Lasting Relief with GTOA
Choosing between Epidural Steroid Injections vs Surgery for Back Pain is a big decision, one you shouldn’t have to make alone. At Greater Texas Orthopedic Associates (GTOA), our spine specialists, pain management experts, and neurosurgeons work together to pinpoint the root cause of your pain and design a treatment plan tailored to your lifestyle and goals.
We bring this expertise closer to you with convenient locations across Texas, including Dallas, San Antonio, Houston, Arlington, Beaumont, and Corpus Christi, so you don’t have to travel far for top-tier care.
Spinal surgery is typically a last resort, after conservative and interventional options such as epidural steroid injections have been fully explored. For many patients, these injections provide valuable short-to-intermediate-term relief, giving you time to build strength through physical therapy and other long-term strategies for spine health.
Take the time to discuss your expectations, concerns, and all available options with our team. We’ll lay out the pros and cons—including potential side effects and recovery timelines—so you can make an informed decision without feeling rushed into an invasive, irreversible procedure.
Don’t let chronic back pain dictate your life. Contact Greater Texas Orthopedic Associates today to schedule a consultation and take the first step toward lasting comfort, improved mobility, and a return to the activities you love.



2 Comments
This article was very insightful and easy to read. The information shared here is truly helpful for anyone interested in orthopedic and legal care topics.
Thank you Laura.
We truly appreciate your kind feedback. Our goal is to make orthopedic and legal medical information accessible and helpful for everyone.