What to Expect at Your First Orthopedic Evaluation After an Injury?
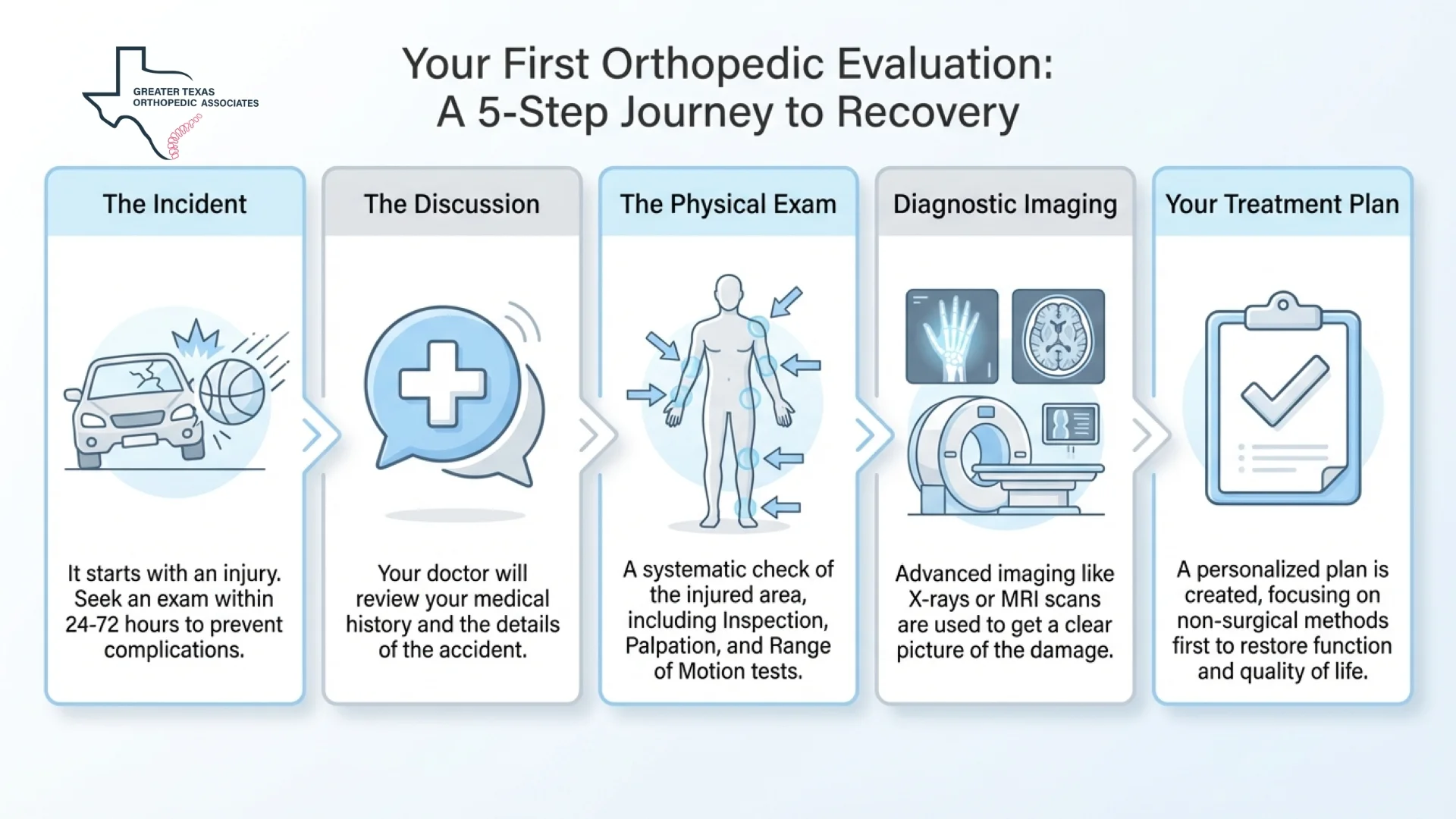
Navigating the aftermath of a physical trauma can be a daunting experience, often characterized by pain, confusion, and uncertainty regarding the future. Whether you have been involved in a motor vehicle collision, a workplace incident, or a sports related trauma, understanding the steps toward recovery is the first priority.
A critical component of your recovery journey is the orthopedic evaluation after injury, which serves as a systematic investigation into the health of your bones, joints, ligaments, tendons, and muscles. This assessment is not merely a check-up; it is a meticulous diagnostic event designed to uncover the root cause of your discomfort and establish a roadmap for your treatment. Because musculoskeletal injuries often have implications beyond localized pain, this evaluation is used to ensure that no occult or hidden injuries are missed.
Why Early Orthopedic Evaluation Matters After an Accident
Following a traumatic event, the human body often enters a state of shock, and the release of adrenaline can temporarily mask significant pain signals. This physiological response may lead some individuals to believe they have escaped serious harm, only to experience debilitating symptoms hours or days later. Seeking an orthopedic exam after accident within the first 24 to 72 hours is essential to ensure that conditions like internal bleeding, fractures, or soft tissue tears are identified before they escalate.
Delaying this initial assessment can result in the injury healing incorrectly, which may permanently limit your strength and range of motion. Furthermore, prompt medical documentation is vital for those navigating insurance claims or legal cases, as it establishes a clear, direct link between the accident and the sustained injuries.
In some injury cases, specialist evaluation are also used for legal and insurance documentation. More information is available on our page about orthopedic evaluations for legal cases.
Reviewing Your Medical History After Injury
The orthopedic assessment process begins with a thorough review of your medical history and the details surrounding your injury. Clinicians typically ask specific questions regarding the mechanism of injury, such as the direction of impact in a car crash or the height of a fall, to help anticipate potential damage. For example, a history of a fall from height may prompt clinicians to investigate concomitant spinal injuries even if the primary complaint is a deformed extremity.
Your symptoms are discussed in detail, including the onset, quality, and location of pain. You should be prepared to describe whether the pain is sharp, dull, burning, or accompanied by sensations like “pins and needles”. Understanding pre-existing health status, including any history of malignancy or conditions such as osteoporosis, helps clinicians determine whether a patient is at higher risk for certain types of fractures.
What Happens During the Physical Examination
The physical portion of the post-injury clinical assessment is a systematic “once-over” that compares the injured area with the healthy side of your body. A structured “look, feel, move, function” methodology is used to ensure a complete assessment.
Inspection and Observation
During the initial stage, the skin is inspected for swelling, discoloration, and visible deformities. Posture and alignment are observed, looking for signs of muscle wasting, which can often accompany joint issues. For instance, asymmetry in the thigh muscles may indicate underlying knee arthritis or chronic dysfunction. Gait is assessed by evaluating the swing and stance phases as you walk, to determine if you are attempting to “unload” a painful limb.
Palpation and Tenderness
The examination then proceeds to palpation, where clinicians gently press on different areas to check for tenderness, abnormal masses, or warmth that may indicate inflammation. Systematic palpation is critical because the pain of a fracture or dislocation can sometimes be referred to another area of the body. Crepitus is also assessed, which is a palpable or audible grinding sensation that occurs as a joint moves.
Range of Motion Testing
Testing your range of motion involves two distinct steps: active and passive movement.
Active movement is the range you can achieve on your own, while passive movement is the range reached when the joint is gently guided by the examiner. A significant difference between the two, where you cannot move the joint yourself but it moves easily when guided, often suggests a soft tissue problem like a tendon tear rather than a joint-specific issue.
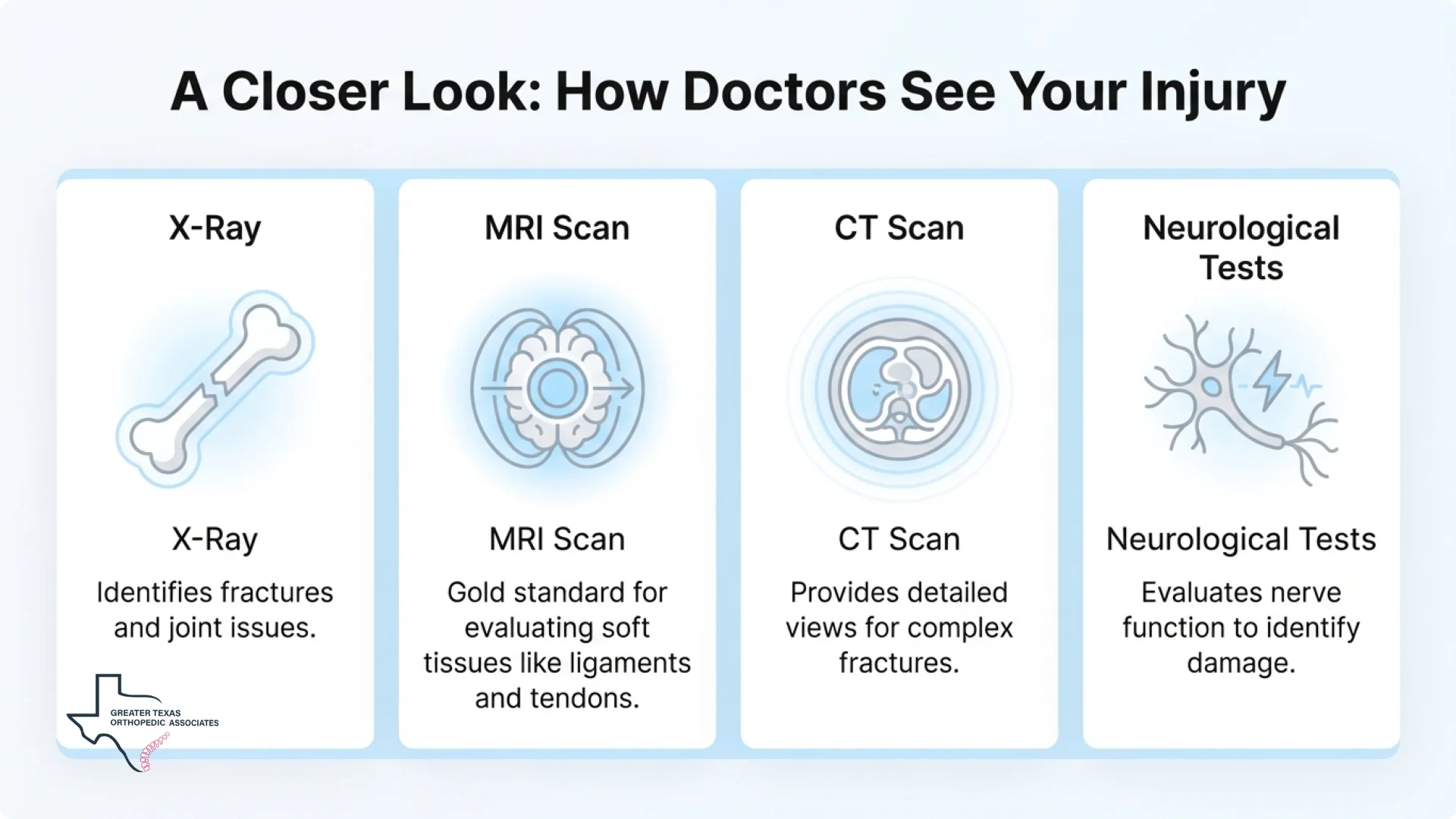
Imaging and Diagnostic Tests Used in Orthopedic Exams
While a physical examination provides the foundation, imaging studies are often necessary to provide a definitive picture of the damage. The orthopedic exam after accident frequently involves a combination of the following tools:
- X-Rays: These are typically the first-line imaging test used to identify bone fractures, dislocations, or joint narrowing. They are quick and effective for monitoring the healing process over time.
- MRI Scans: Magnetic Resonance Imaging is the gold standard for evaluating soft tissues like ligaments, tendons, and discs.
- CT Scans: These provide detailed cross-sectional views of the body, which are invaluable for diagnosing complex fractures or internal organ damage that may not be visible on a standard X-ray.
- Ultrasound: This non-invasive tool is used to assess abdominal trauma and soft tissue injuries, and it is frequently used to guide therapeutic injections.
- Neurological Testing: If you experience numbness or weakness, EMG or Nerve Conduction Velocity (NCV) tests may be used to evaluate nerve function and identify potential nerve damage.
The Orthopedic Assessment Process in Specific Injuries
The trauma-related assessment varies slightly depending on the region of the body affected. Because orthopedic injuries can affect the body from head to toe, specialists tailor the evaluation to the specific type and location of trauma.
Spinal and Back Injuries
Vehicle collisions frequently result in spinal trauma, including whiplash, herniated discs, or fractures. Back pain is classified by its duration (acute, subacute, or chronic) and its location (lumbar, thoracic, or cervical) to determine the best treatment pathway.
Extremity and Joint Trauma
Injuries to the arms, legs, hands, and feet can range from simple sprains to complex open fractures. Joint stability is evaluated, and clinicians check for signs of conditions such as frozen shoulder or ligament tears in the knee.
If you are struggling with persistent joint pain after an injury, [facet joint injection] is a type of interventional procedure we may consider to provide both a diagnosis and relief.
Understanding Orthopedic Care for Accident Injuries
Once a diagnosis is established, we develop a personalized treatment plan aimed at restoring your function and quality of life. The goal of orthopedic care for accident injuries is always to prioritize conservative, non-surgical methods whenever possible.
Conservative Management
Most musculoskeletal injuries respond well to non-invasive strategies. These include:
- Physical Therapy: A cornerstone of rehabilitation that focuses on strengthening supporting muscles and improving flexibility.
- Medication Management: Anti-inflammatory medications or muscle relaxants may be prescribed to reduce swelling and relieve pain.
- Immobilization: Using casts, braces, or splints allows bones and soft tissues to heal in the proper alignment.
Interventional Pain Management
When conservative measures are insufficient, targeted interventional options may be considered for nerve and joint pain. For instance, [Epidural Steroid Injections] are used to reduce nerve inflammation in cases of sciatica or herniated discs. Another advanced option is [Radiofrequency Ablation], which uses heat to deactivate nerves responsible for chronic pain.
Surgical Intervention: When Is It Necessary?
In some cases, the orthopedic evaluation after injury reveals damage that cannot be repaired through conservative means. Surgery may be necessary for displaced fractures, complete ligament tears, or severe spinal instability. Minimally invasive surgical techniques, such as arthroscopy or microdiscectomy, are often used to reduce recovery time and minimize muscle damage.
Surgical goals typically include realigning fractures, repairing vascular damage, and stabilizing the spine to restore function. Even when surgery is required, orthopedic specialists work alongside Neurosurgery and pain management teams to provide a holistic recovery plan.
The Role of Medical Documentation in Legal and Insurance Contexts
Beyond diagnosis and treatment, an injury-focused evaluation also generates detailed medical documentation that may play an important role in insurance claims or personal injury cases. These records help establish the nature of the injury, its connection to the accident, and the medical necessity of ongoing care.
In legal and insurance settings, well-documented timelines, objective findings, and clearly stated prognoses are often used to support claim evaluations and case decisions. This is particularly relevant in injury cases where treatment extends over time or symptoms evolve after the initial trauma.
For a deeper discussion of how orthopedic documentation is used within personal injury cases, see our related article: [How Lien Doctors Strengthen Personal Injury Cases]
What You May Feel During the Evaluation?
It is natural to feel some anxiety before your first visit. During the orthopedic exam after accident, we strive to maintain your comfort. You might feel mild pressure as we guide your joints or a brief “pinch” if a local anesthetic is used for a diagnostic injection.
We encourage you to communicate openly throughout the orthopedic assessment process. If any movement causes sharp pain, let us know immediately, as this is a valuable clinical clue that helps us narrow down your diagnosis. Most patients find that the clarity provided by a definitive diagnosis far outweighs any temporary discomfort during the evaluation.
Long-Term Outcomes and The Path to Recovery
The final stage of the injury-focused evaluation steps is the transition from diagnosis to active rehabilitation. We provide ongoing monitoring to ensure your healing is progressing as expected and to adjust your treatment plan as you gain strength. For many, the goal of orthopedic care for accident injuries is a return to work and daily activities without persistent pain.
Recovery is often a gradual process, like reinforcing the foundation of a house; we focus on stabilizing the injury first, then strengthening the body to prevent future stress. With the right team and a structured plan, achieving a pain-free, active life is a reachable goal.
Conclusion
Your first orthopedic evaluation after injury is the most significant step you can take toward reclaiming your health and mobility. By combining board-certified expertise with advanced diagnostic technology, we ensure that your injuries are identified accurately and treated effectively. Whether your path involves conservative therapy, interventional pain relief, or specialized surgery, the GTOA team is here to support you through every stage of your recovery journey.
Timely evaluation and appropriate care play an important role in long-term recovery and functional outcomes. If you or a loved one needs expert orthopedic care for accident injuries, reach out to GTOA today to schedule your consultation. Our commitment to medical precision and compassionate care ensures that you have the strongest possible foundation for your health and your legal future.