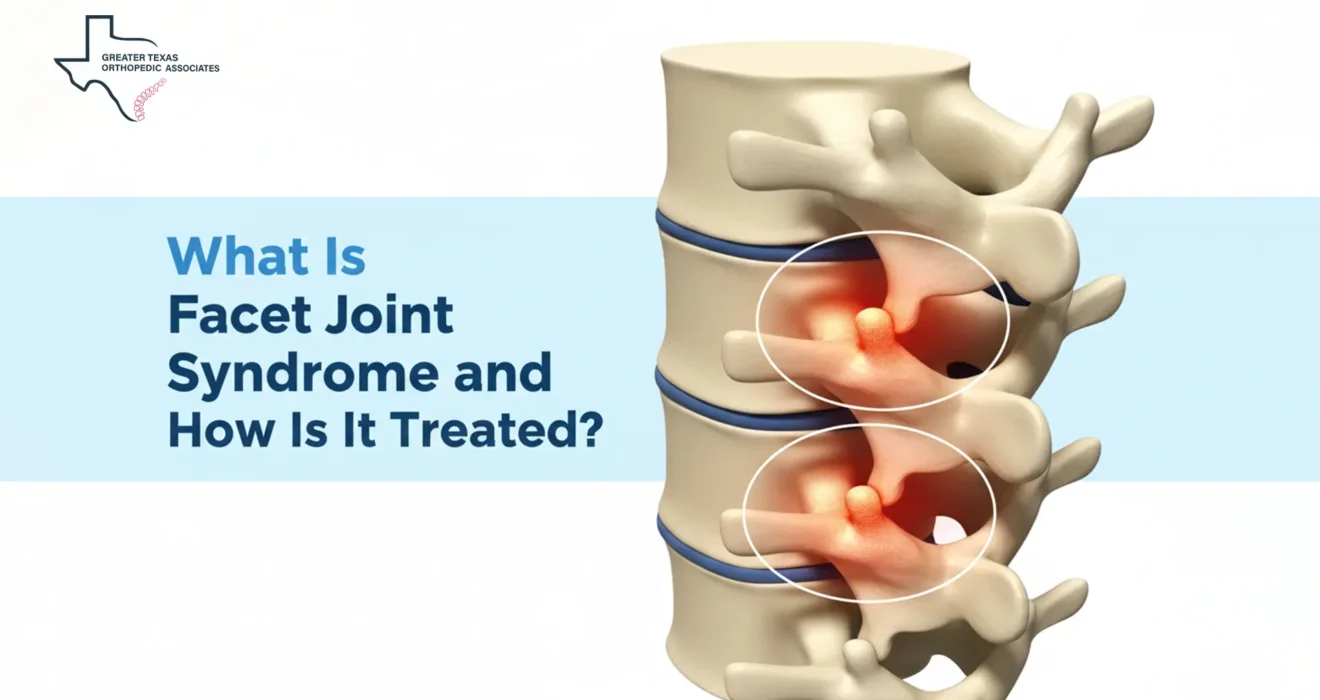
What Is Facet Joint Syndrome and How Is It Treated?
Facet joint syndrome is one of the most common sources of persistent neck and back pain. This degenerative condition affects millions of people, gradually limiting mobility, flexibility, and the ease of performing everyday activities. Although the joint damage itself cannot be reversed, a wide range of conservative treatments, image-guided injections, and surgical options can significantly reduce pain and improve long-term function. A clear understanding of this condition begins with the anatomy of the facet joints and the mechanical changes that trigger its characteristic symptoms.
Understanding the Facet Joints
To comprehend what is Facet Joint Syndrome, one must first appreciate the role of the facet joints themselves. The spine, a complex structure made of connected and movable bones known as vertebrae, relies on these joints to maintain stability and facilitate movement.
Between each vertebra, a disc and two facet joints form a crucial three-joint complex. Facet joints, also referred to as zygapophysial joints, are classified as synovial joints. They possess a fibrous capsule encompassing the bone and articulating cartilage, and they contain synovial fluid lubrication and a cartilage lining.
This specialized structure allows the vertebrae to slide, glide, bend, and twist fluidly, while simultaneously limiting excessive rotation to prevent the bones from slipping over each other. The medial branch of the dorsal spinal ramus acts as the sensory nerve for these joints, transmitting pain signals to the brain when irritation or inflammation occurs.
This syndrome is characterized as an arthritis-like spine condition wherein one or more of these crucial joints become a source of chronic pain.
What causes facet joint syndrome? Etiology and Risk Factors
The most common underlying factor leading to facet joint problems is the degeneration of the spine, often referred to as spondylosis. This process involves the natural progression of wear and tear, eventually leading to osteoarthritis (OA) of the joints. As degenerative changes occur in the spinal column, the body’s weight distribution can shift unevenly, placing excess pressure on the facet joints.
This additional mechanical stress causes the joint capsules to thin and the smooth cartilage to gradually break down. Over time, new bone formation, known as osteophytes or bone spurs, may develop around the joint, and the joint itself becomes irritated and inflamed.
While degeneration is the primary issue, what causes facet joint syndrome can be influenced by several compounding risk factors:
- Age: Most common in adults between 40 and 70, particularly over 50.
- Obesity: Extra weight increases stress on the joints.
- Trauma or Injury: Past injuries like whiplash or spinal fractures raise the risk.
- Lifestyle: Poor posture, sedentary habits, or repetitive twisting movements can exacerbate joint stress.
This syndrome is therefore primarily a mechanical problem worsened by age and physical stress.
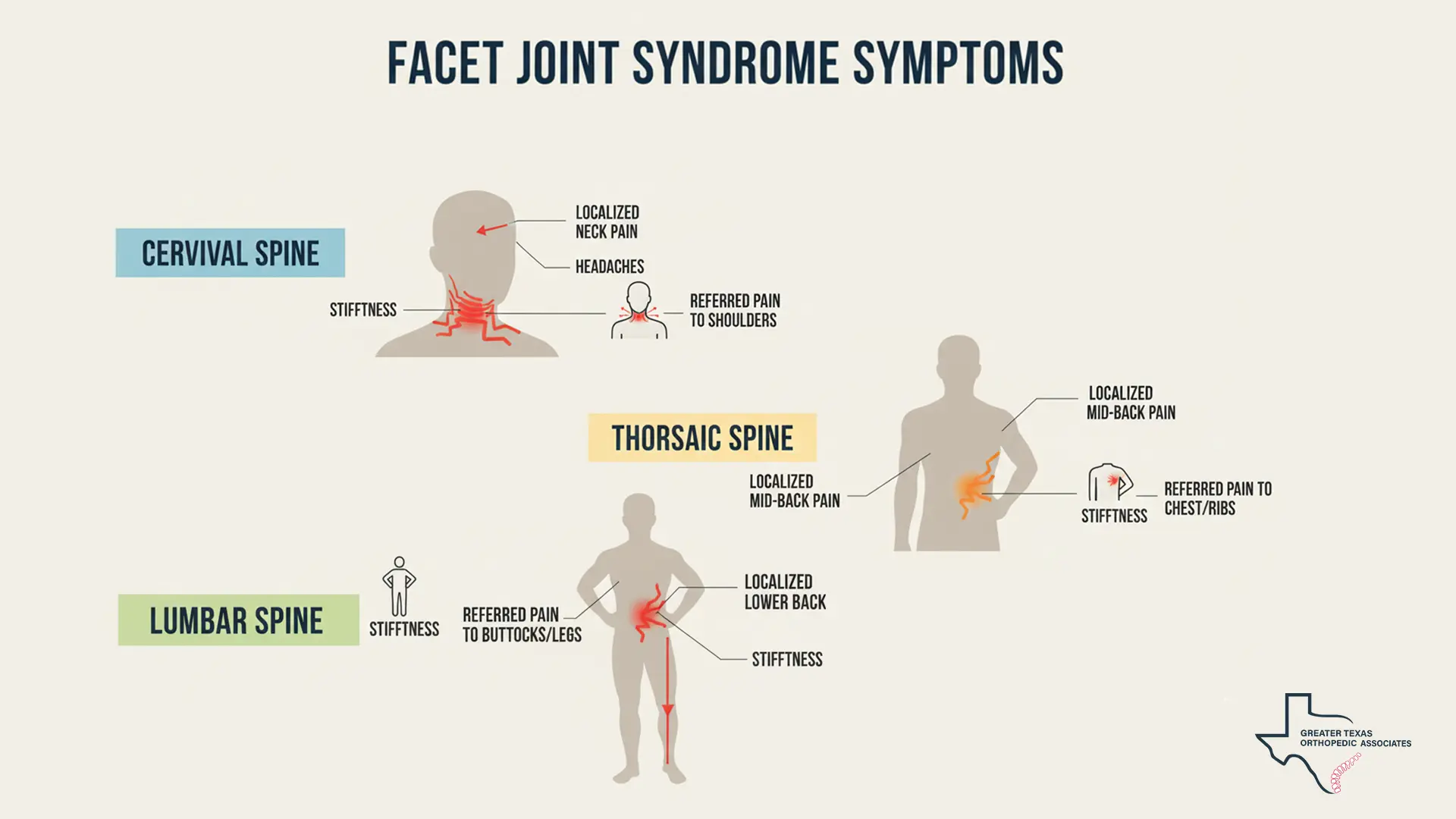
Facet Syndrome Symptoms and Their Locations
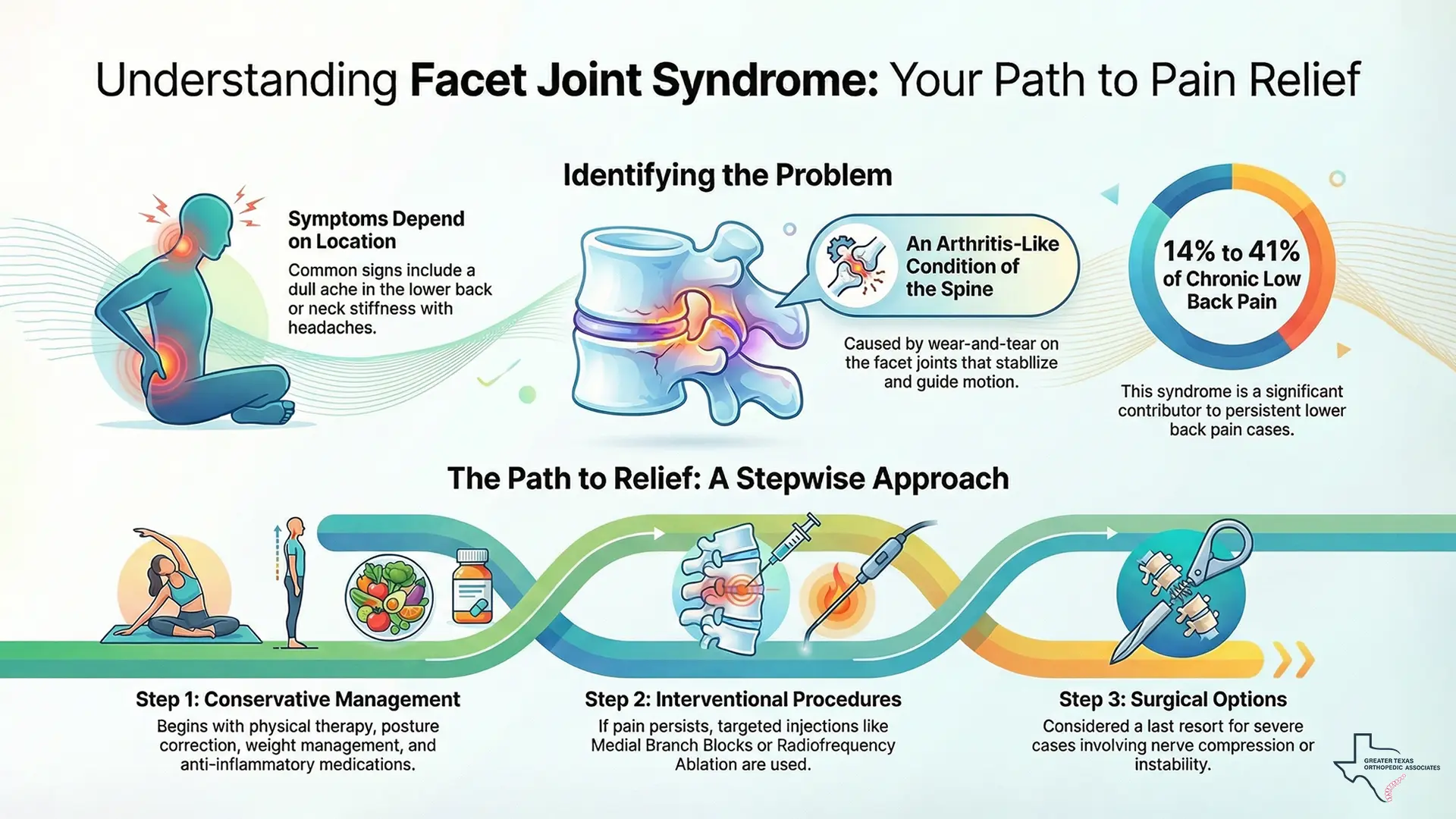
The clinical presentation and location of Facet Syndrome Symptoms depend on whether the damaged facet joints are in the lumbar spine (lower back), the cervical spine (neck), or, less commonly, the thoracic spine (mid-back).
Lower Back (Lumbar Region)
In the lumbar region, where the spine bears most of the body’s weight, facet joint problems are a common contributor to chronic lower back pain, accounting for 14% to 41% of cases.
Common Facet Syndrome Symptoms associated with lumbar involvement include:
- Localized Dull Ache: Pain felt directly over the lower spine.
- Referred Pain: Pain may radiate to the buttocks, hips, thighs, or knees (“pseudo-radicular” pain without nerve damage).
- Pain with Movement or Sitting: Bending backward, twisting, or prolonged sitting often worsens discomfort.
- Relief with Forward Movement: Bending forward or changing positions can ease the pain.
Since facet-related lumbar pain often overlaps with symptoms caused by disc pathology, such as referred pain or discomfort with prolonged sitting, patients may benefit from reviewing our comprehensive article on [Lumbar Disc Herniation], which explains how disc problems differ from facet-mediated pain.
Neck and Mid-Back (Cervical and Thoracic Regions)
Degeneration in cervical or thoracic facet joints can cause:
- Neck Pain and Stiffness: Pain at the base of the skull, neck, and shoulders, limiting head movement.
- Headaches: Often originating from irritated joints.
- Radiating Pain: Pain may spread to the shoulders, upper, or mid-back.
If bone spurs develop, they can press on nerves, causing sharp, radiating pain, numbness, weakness, or tingling in arms or legs. Severe stiffness may make standing upright difficult or lead to a hunched posture.
Diagnosing Facet Joint Syndrome
Facet joint problems can mimic other spinal conditions, making diagnosis challenging. It begins with a thorough clinical evaluation, including medical history, physical examination, and pain assessment. During the exam, a physician may move the patient in various positions, such as bending backward or twisting the torso (Kemp’s maneuver), to pinpoint the source of pain.
Imaging tests like X-rays, CT scans, or MRI can help identify joint degeneration, narrowing, or bone spurs, and rule out other conditions such as disc herniation or fractures. However, imaging alone doesn’t always correlate with the patient’s pain, as degeneration can occur without symptoms.
The most reliable method to confirm facet joint pain is the diagnostic Medial Branch Block (MBB). This involves injecting a local anesthetic near the medial branch nerves that carry pain signals from the joints. If the patient experiences significant temporary relief, usually at least 50%, the facet joint is confirmed as the pain source. To ensure accuracy, doctors often repeat the MBB on a separate occasion before planning long-term treatment.
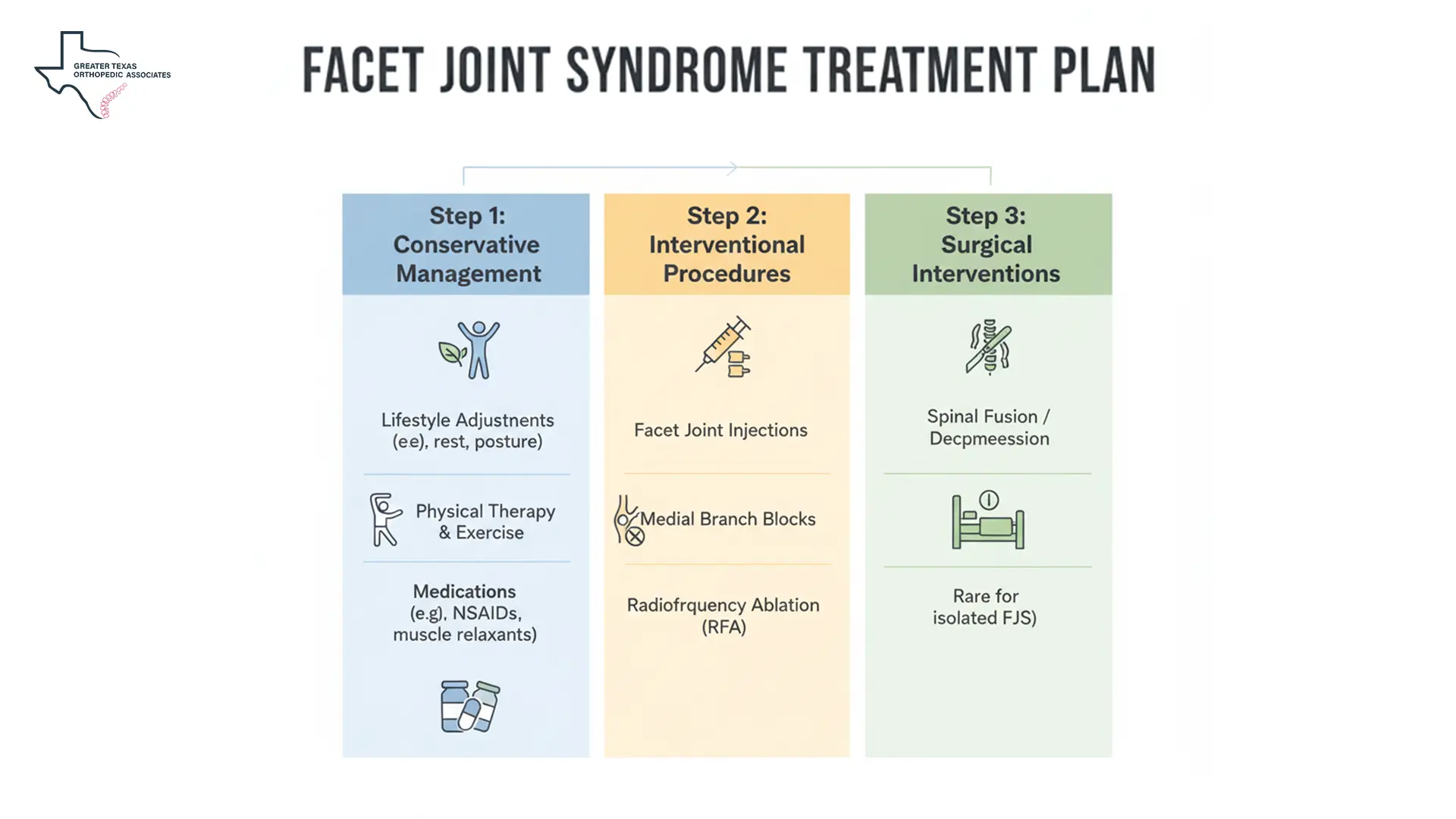
How to Treat Facet Joint Syndrome: A Stepwise Approach
For patients wondering what these syndromes are and how they impact their mobility, it is crucial to understand that while the condition is chronic and progressive, the pain associated with it can be effectively managed. Treatment for this condition involves a structured, stepwise approach that begins with the least invasive options and progresses to interventional procedures and, finally, surgery, if necessary.
Step 1: Conservative Management (First-Line Treatments)
This degenerative problem is chronic and progressive, but pain can often be managed with non-invasive strategies that reduce stress on the spine and improve mobility.
1. Lifestyle Adjustments & Self-Care
- Weight Management: Losing weight decreases pressure on the facet joints, reducing pain and slowing degeneration.
- Proper Posture: Sitting and standing correctly keep the spine aligned. Desk workers benefit from chairs with straight backs and armrests.
- Heat & Cold Therapy: Heat relaxes muscles and eases stiffness, while cold therapy reduces inflammation during flare-ups.
- Back Brace: Supports the spine and limits motion, reducing joint pressure when needed.
2. Medications & Physical Therapy
- Medications: Oral NSAIDs, topical creams or patches, and sometimes muscle relaxers relieve pain and stiffness.
- Physical Therapy & Exercise: Stretching, strengthening, and low-impact activities like walking improve flexibility, core stability, and posture, reducing pressure on facet joints.
Step 2: Interventional Procedures (Targeted Pain Relief)
When conservative therapies fail to provide adequate long-term relief, targeted, minimally invasive procedures are the next step in determining how to treat facet joint syndrome. These methods aim to directly reduce inflammation or block specific nerves that transmit pain signals.
For patients seeking personalized care, we at GTOA offer advanced interventional pain management techniques, providing accurate diagnoses and customized treatment plans for lasting relief.
1. Facet Joint Injections (FJIs)
Facet joint injections serve both diagnostic and therapeutic purposes. A combination of local anesthetic (for immediate numbing) and corticosteroid (for longer-term inflammation reduction) is injected directly into the facet joint capsule. Relief can last from weeks to months, allowing patients to focus on physical therapy and strength-building. This procedure is minimally invasive and usually performed outpatient basis.
For chronic spinal pain, obtaining a Comprehensive Injury Assessment is a crucial step to identify the exact structural issues, like facet joint degeneration, driving the discomfort.
For patients wanting a detailed breakdown of how the procedure works and what to expect, our dedicated page on Facet Joint Injections provides step-by-step guidance and treatment information.
2. Medial Branch Blocks (MBBs)
Medial Branch Block (MBB) are primarily diagnostic, injecting an anesthetic near the medial branch nerves. A successful block helps predict the efficacy of longer-term treatments.
3. Radiofrequency Ablation (RFA)
If the diagnostic MBBs confirm that the facet joints are the source of pain, Radiofrequency Ablation (RFA), also known as Endoscopic Rhizotomy, is often the recommended next step for long-term relief.
RFA is a minimally invasive procedure that uses heat generated by radio waves to target and destroy (cauterize) the medial branch nerves, interrupting their ability to transmit pain signals to the brain. This process does not eliminate what is Facet Joint Syndrome. But rather eliminates the pain caused by it.
RFA can provide sustained relief, typically lasting from six months up to one year, or even longer in some cases, because the nerve must regenerate before pain returns. If pain eventually returns, the procedure can often be safely repeated.
For readers interested in a deeper understanding of this cutting-edge pain management procedure, specifically comparing it to other injection methods, please consult our detailed resource on [Medial Branch Blocks vs. Facet Joint Injections]
Step 3: Surgical Interventions (The Last Resort)
Surgery is generally considered only when non-surgical treatments fail or when there are severe neurological symptoms or structural instability. While it cannot reverse facet joint degeneration, surgery can reduce pain and improve functionality.
Common surgical options include:
- Lumbar Spinal Fusion: Fuses two or more vertebrae to eliminate motion, stabilizing the segment and reducing pain from instability.
- Facetectomy: Removes bone spurs within the facet joints (a key component of what causes facet joint syndrome) to relieve nerve compression.
- Laminectomy (Lumbar Decompression): Removes part of a vertebra to create space for nerves, often recommended if spondylolisthesis is present.
- Discectomy: Removes damaged disc material, compressing nerves around the facet joint.
Surgery is typically reserved for specific structural problems or intractable pain. Modern techniques, such as Minimally Invasive Spine Surgery (MISS) and endoscopic procedures, aim to minimize muscle damage, reduce post-operative pain, and speed up recovery.
Prognosis and Long-Term Management
This pain-generating problem is a progressive, chronic condition, meaning degeneration typically advances with age. Complete pain resolution isn’t always possible, but interventional procedures combined with ongoing non-surgical care can make pain manageable and improve quality of life.
Long-term management focuses on preventing progression and maintaining function:
- Consistent Exercise: Regular physical therapy and core strengthening stabilize the spine and reduce stress on facet joints.
- Healthy Lifestyle: Maintaining a healthy weight and balanced diet helps lower joint stress and inflammation.
With specialized diagnosis and a tailored plan for how to treat facet joint syndrome, patients can achieve lasting relief and stay active despite the chronic nature of the condition.
Conclusion
What Is Facet Joint Syndrome? It’s a common, chronic, arthritis-like spinal condition caused by degenerative wear and tear on the facet joints, often accelerated by aging, obesity, or past trauma. Inflammation and cartilage breakdown cause characteristic Facet Syndrome Symptoms, including stiffness and dull, axial back pain that worsens with extension and rotation. Accurate diagnosis often requires clinical evaluation and procedures like Medial Branch Blocks.
While degenerative changes are permanent, aggressive treatment is available. The strategic determination of how to treat facet joint syndrome follows a stepwise approach, from non-invasive strategies like weight loss and targeted exercise to interventional injections (FJIs, RFA), and, in rare cases, surgery to correct structural issues or relieve nerve compression. With a skilled medical team and a personalized long-term plan, patients can achieve improved mobility and a significant reduction in chronic pain.