Neck Disc Problems: Causes, Symptoms, and Treatment Options
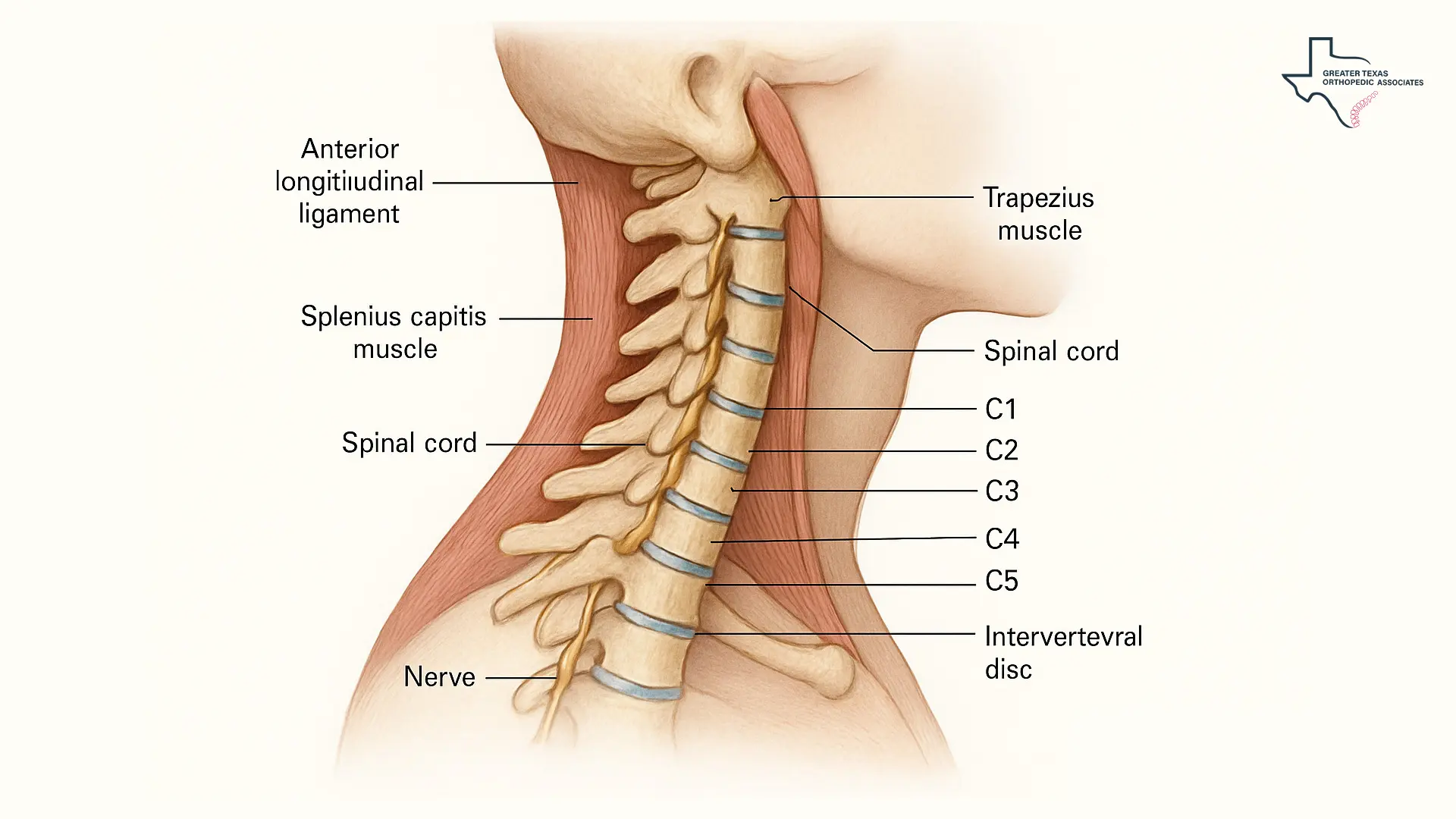
The cervical spine, located in the neck region, is a complex structure consisting of seven vertebrae cushioned by intervertebral discs. These discs are vital components, acting as shock absorbers, providing cushioning for the vertebrae, and ensuring flexibility for movements like twisting, turning, bending, and running.
When these essential structures are damaged by injury or age-related wear, it can lead to neck disc problems that significantly impact an individual’s mobility, quality of life, and overall health. Understanding the root causes, recognizing the symptoms, and exploring modern neck pain treatment options are the critical first steps toward finding lasting relief.
At GTOA, our multidisciplinary team of specialists provides patients across Texas with expert evaluations and personalized treatment plans for neck disc problems and related cervical spine conditions. By combining expertise across multiple disciplines, we ensure comprehensive care tailored to each patient’s specific symptoms and needs.
Cervical Disc Anatomy: Structure and Function
The spine is a flexible column of bones that protects the spinal cord, stretching from the base of the skull to the tailbone. The neck region, known as the cervical spine, houses the top seven vertebrae (C1-C7). Situated between these vertebrae are the cervical discs, which are composed of two distinct layers:
- Annulus Fibrosus: This is the sturdy, protective outer layer constructed of concentric collagen fibers. This layer is strong enough to shield the soft inner core and helps handle the spine’s heavy loads and absorb shocks.
- Nucleus Pulposus: Located in the center, this gel-like interior is protected within the annulus fibrosus. It provides additional cushioning and flexibility necessary for neck movements.
When the outer layer (annulus fibrosus) weakens or tears, the inner gel-like substance (nucleus pulposus) can push out. This is how a disc becomes damaged or “herniated,” leading to various neck disc conditions.
Causes of Neck Disc Problems and Risk Factors
Problems affecting the cervical discs are typically caused by age-related changes, but they can be accelerated or triggered by specific factors:
- Degeneration and Aging: The primary cause of neck disc disease is the natural aging process. As people age, the discs lose hydration and water content, causing them to become less jelly-like, stiffer, and prone to wear and tear. This weakening reduces their ability to cushion the spine, making them vulnerable to tearing or rupturing.
- Trauma or Injury: Sudden, jarring motions, injuries, or trauma to the cervical spine, such as those sustained in an accident, can cause immediate damage to the intervertebral discs and accelerate degeneration.
- Poor Posture and Repetitive Strain: Maintaining poor posture, particularly when sitting for extended periods, or engaging in repetitive motions like bending, twisting, or lifting heavy objects, can place additional stress on the cervical discs, leading to increased wear and tear.
- Genetics and Lifestyle: Some individuals may be genetically predisposed to developing disc problems. Unhealthy habits, such as chronic smoking, can impair the delivery of oxygen and nutrients to the discs, causing them to degenerate more quickly.
Common Cervical Disc Conditions: Herniation & Degeneration
Damage to the cervical discs often manifests in two primary ways: Cervical Degenerative Disc Disease (DDD) and cervical disc herniation.
Cervical Degenerative Disc Disease (DDD)
DDD refers to the condition where the cervical discs thin and lose elasticity over time, reducing their ability to absorb shock. As the discs lose height, the vertebrae move closer together. The body may attempt to stabilize the area by forming extra bone, known as bone spurs (osteophytes), around the disc. These bone spurs can narrow the small openings (foramina) where nerve roots exit, leading to nerve compression, a condition called foraminal stenosis. DDD is a general term for age-related wear and tear in the neck.
Cervical Disc Herniation
A cervical disc herniation occurs when the sturdy outer layer (annulus fibrosus) tears, and the soft, gel-like inner core (nucleus pulposus) leaks or bulges out into the tear. This condition is also known as a prolapsed or slipped disc. The pain is typically caused when the inner material, which contains inflammatory proteins, leaks onto or presses against a nearby nerve root. Less commonly, a herniated disc may compress the spinal cord itself. A herniated cervical disc is more common in people up to 50 years old.
Symptoms of Cervical Disc Problems: Pain, Numbness, Weakness
The symptoms of these problems vary widely, ranging from mild aching to severe, electric-like pain and neurological deficits, depending on which nerve root or spinal segment is affected.
Localized and Radiating Pain
The most common symptoms include chronic neck pain, which may be dull, aching, or sharp, and stiffness that makes it difficult to turn the head. This discomfort can be localized or may radiate to the shoulders, arms, and hands. The pain from a slipped disc in the neck often affects only one arm. Moving the neck in certain ways, such as extending or straining it, may increase the pain.
Neurological Symptoms (Radiculopathy)
When a nerve root in the neck becomes compressed and inflamed, it leads to cervical radiculopathy, or a “pinched nerve”. Since the nerves that connect to the cervical spine extend to the shoulders, arms, chest, and upper back, neurological symptoms can radiate down to these areas. These symptoms include:
- Numbness and Tingling: A “pins and needles” feeling in a shoulder or arm that may extend down to the fingers.
- Muscle Weakness: Weakness in the arms, hands, and fingers, which can make it difficult to grip objects or perform fine motor tasks.
- Weakened Reflexes: A decrease in the normal reflex responses.
- Sharp or Burning Pain: The pain is often described as sharp or burning in nature.
Severe Symptoms (Myelopathy)
If the disc or bone spurs compress the spinal cord itself, this is a serious condition known as myelopathy (spinal cord dysfunction). Myelopathy can have profound effects, including impaired walking and coordination. Symptoms of myelopathy include:
- Gait Disturbances: Difficulty with walking, often manifesting as an unsteady walk, stiffness, jerkiness, or stumbling.
- Loss of Balance: Disruption of proprioception (the body’s ability to sense its position in space), making maintaining balance challenging.
- Loss of Bowel and/or Bladder Control: These are rare but possible and dire outcomes of spinal cord compression.
If neurological symptoms like progressive weakness, difficulty walking, or loss of bowel/bladder control are present, immediate medical attention is required to prevent the symptoms from worsening or becoming permanent.
How Cervical Disc Problems Are Diagnosed
Diagnosing the source of cervical disc issues begins with a thorough evaluation by a specialist. The diagnostic process typically includes:
Physical Examination:
A healthcare provider will review the patient’s medical history and symptoms, then examine the neck, shoulders, arms, and hands, checking for muscle weakness, changes in reflexes, and comparing sensations on both sides of the body. Certain neck movements may be performed to try and recreate or relieve symptoms.
Imaging Tests:
Imaging is vital for confirming a diagnosis or ruling out other conditions.
- X-rays: Useful for assessing neck and arm pain; they can show disc-space narrowing or foraminal stenosis.
- MRI: The preferred method for evaluating radiculopathy, providing detailed images of soft-tissue problems like disc protrusion or nerve compression.
- CT Scan: Often used after trauma, offering clear cross-sectional views of the spine.
- EMG: Measures muscle electrical activity to determine whether the nerves are functioning properly.
Neck Disc Treatment Options: Conservative to Surgical
Conservative Management
The initial approach to treatment for neck pain focuses on reducing inflammation, relieving pain, and improving mobility, often yielding good-to-excellent outcomes in about 90% of cervical radiculopathy cases.
- Rest and Activity Modification: Modifying activities to avoid painful movements is crucial until pain subsides. Maintaining good posture and a healthy weight can also help slow the progression of degenerative disc disease.
- Medication: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, muscle relaxants, and sometimes short courses of oral corticosteroids are prescribed to reduce inflammation and muscle spasms caused by nerve compression.
- Physical Therapy (PT): A tailored PT program is a cornerstone of therapies for neck pain. Exercises focus on strengthening the neck and shoulder muscles, improving the range of motion, and enhancing balance. Pain relief from an injection often “unlocks” the ability to participate in these crucial strengthening exercises.
- Immobilization: In some instances, wearing a soft cervical collar (neck brace) may be recommended for short-term management (one to two weeks) to minimize movement and reduce nerve root irritation.
Interventional Pain Management
When conservative measures fail to provide adequate relief after several weeks or months, targeted, minimally invasive injections may be used to address chronic pain. Before moving forward with any injection or surgical option, obtaining a clear diagnosis is crucial. Our team offers specialized Comprehensive Injury Assessments to pinpoint the exact source of your pain.
Epidural Steroid Injections (ESIs): An ESI involves injecting a potent anti-inflammatory corticosteroid, often combined with a local anesthetic, directly into the epidural space surrounding the inflamed spinal nerves. ESIs are commonly used for conditions like cervical disc displacement and spinal stenosis, where nerve inflammation is the primary source of pain. While they do not cure the underlying structural issue, they lessen swelling and relieve pain, sometimes lasting for several weeks to several months. ESIs are a common component of a comprehensive approach to neck pain treatment.
Facet Joint Injections (FJIs): Facet joints (small joints at the back of each vertebra) can be a significant source of neck pain due to arthritis or degeneration. Facet joint injections deliver local anesthetic and/or corticosteroids directly into the joint capsule, serving both diagnostic and therapeutic purposes.
Medial Branch Blocks (MBBs) and Radiofrequency Ablation (RFA): MBBs are diagnostic injections used to confirm if the facet joints are the source of pain. If a block is successful, the next step is often Radiofrequency Ablation (RFA), a minimally invasive procedure that uses heat to deactivate the specific nerves sending pain signals. RFA can provide longer-lasting relief, often for six months to a year or longer.
📌For a deeper look at how medial branch blocks compare to other injection-based options, you can explore our detailed guide on [medial branch blocks vs. facet joint injections]
Surgical Intervention
Surgery is generally considered a last resort, recommended when non-surgical treatments fail to provide adequate relief after at least six to 12 weeks, or when a patient experiences severe or worsening neurological deficits, such as progressive weakness or loss of coordination.
- Cervical Discectomy and Fusion: These procedures aim to relieve pressure on the spinal cord or nerve roots. Spinal fusion joins two or more vertebrae to stabilize the spine.
- Cervical Disc Replacement (CDR): CDR is an alternative to fusion that alleviates nerve pressure while preserving spinal mobility.
- Minimally Invasive Spine Surgery (MISS): Utilizing specialized tools and smaller incisions, MISS procedures, like microdiscectomy, are designed to reduce tissue damage, minimize post-operative pain, and facilitate a quicker recovery time.
Neurosurgical specialists focus on procedures for the spine and nervous system, including surgical management of spinal cord compression and specialized treatments for herniated discs.
Conclusion
Neck disc problems, including cervical degenerative disc disease and cervical disc herniation, stem from wear and tear of the cervical spine, often causing chronic pain and neurological symptoms in the arms and hands. Early recognition of warning signs, such as weakness or gait issues, is crucial to prevent worsening.
A wide range of neck pain treatment options exists, from conservative approaches like physical therapy and medication to interventional procedures such as ESIs and RFA, and surgical options for severe cases. Consulting a multidisciplinary team ensures a precise diagnosis and a tailored plan to restore mobility, comfort, and overall quality of life.
Managing cervical disc issues is like reinforcing a house’s foundation: the goal is not just temporary relief, but strengthening the spine to withstand future stress. With careful evaluation and a stepwise approach, lasting relief from chronic neck discomfort is achievable.