Understanding Joint Rheumatism: Symptoms, Causes, and Modern Treatments
The path to living comfortably often requires accurately identifying the source of chronic pain, especially when symptoms affect the musculoskeletal system. For many individuals experiencing persistent aches, swelling, and stiffness in their joints, the condition may be broadly referred to as rheumatism. While this is an older term no longer officially used in modern medicine, it generally describes pain and symptoms affecting the muscles and joints, often acting as an informal umbrella term for over 100 health conditions that cause joint damage or pain, such as rheumatoid arthritis and osteoarthritis.
At GTOA, we are dedicated to providing specialized orthopedic healthcare services and pain management for individuals suffering from significant injuries and chronic conditions. Our experienced team combines advanced diagnostics with effective treatment strategies to accurately diagnose the root cause of musculoskeletal pain and restore function. For more information about how our team of specialists can help you, we invite you to visit our Contact Us page to schedule a consultation.
What is joint rheumatism?
To answer this fundamental question, we must first clarify the terminology. The word “rheumatism” itself is not a specific medical condition or diagnosis. In clinical practice, the focus shifts to specific rheumatic diseases, which number around 200 and affect the joints or connective tissue. Often, when people use this word, they are actually referring to rheumatoid arthritis (RA).
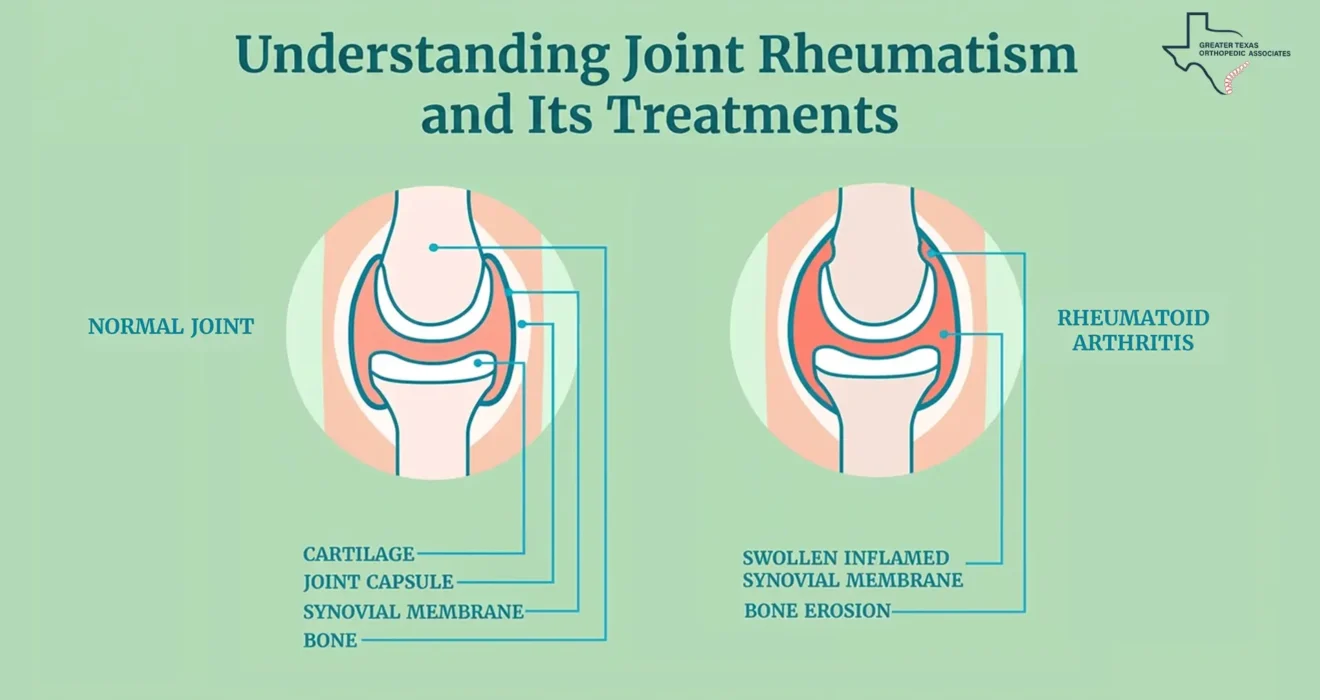
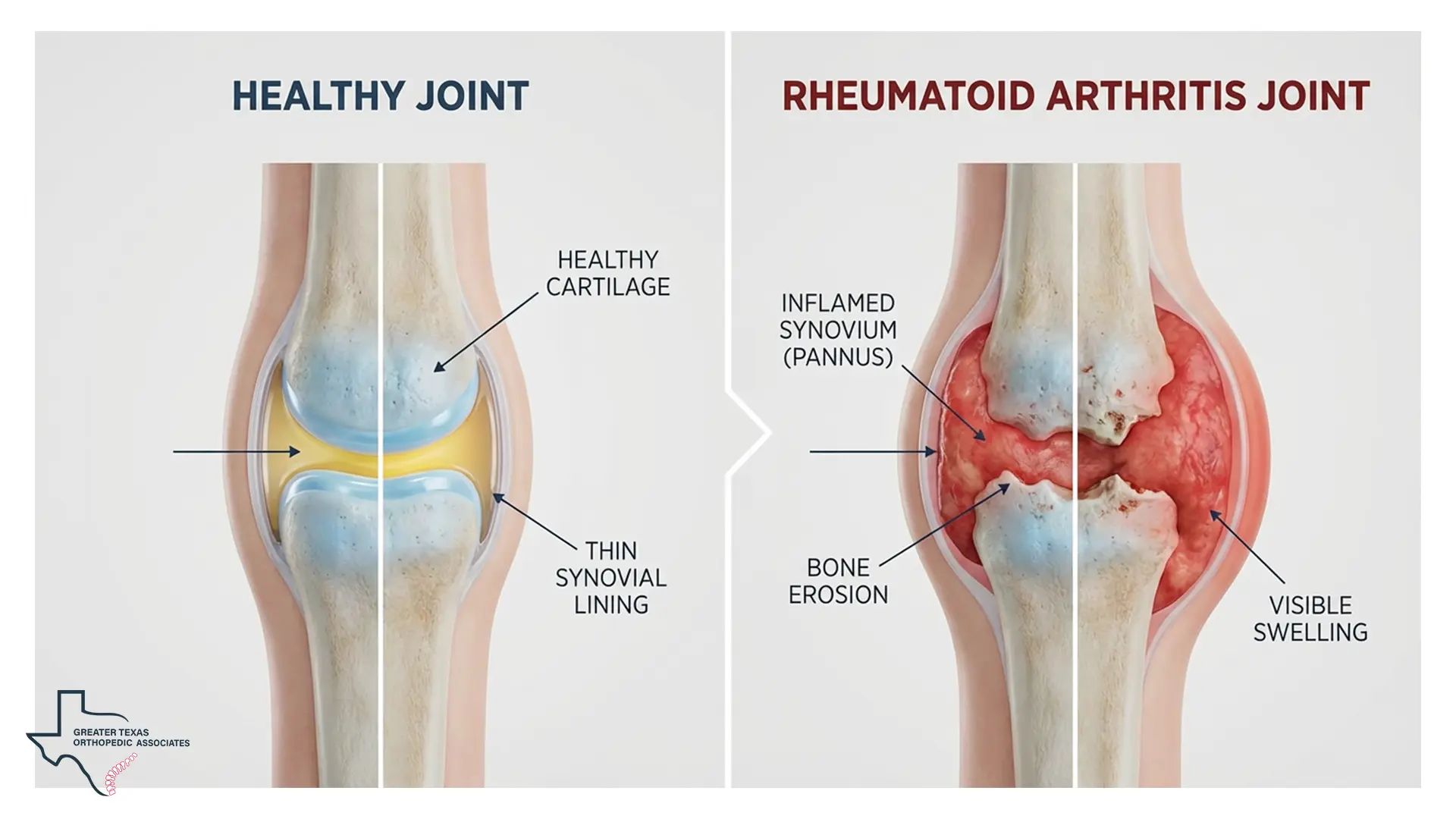
This condition is a chronic, autoimmune disease that causes pain, swelling, and stiffness in the synovium, the lining of the joints. This ailment is best characterized as an immune-mediated inflammatory disease (IMID). In such an autoimmune disease, the immune system mistakenly attacks the body’s own tissues, including the synovium.
Unlike osteoarthritis, which results from the wear and tear of joints that often comes with age, this inflammatory condition occurs due to an internal immune system attack. This attack causes the synovium, which normally is a thin lining that provides nutrients and lubrication, to become thickened and inflamed. This thickening often results in a hypertrophied synovium, referred to as pannus, which invades and erodes adjacent cartilage and bone.
If left untreated or undertreated, the chronic inflammation and damage can cause the joints to bend out of shape (deformity), leading to severe pain and loss of mobility and function. The damage caused by this form of inflammatory arthritis can progress through four stages, ranging from early inflammation without bone damage (Stage 1) to severe pain, swelling, and eventual fusion of the joints (Stage 4).
Understanding what is joint rheumatism truly means acknowledging that it points toward inflammatory and autoimmune joint conditions like RA, which require specialized, long-term management to stop this destructive process.
Joint rheumatism symptoms
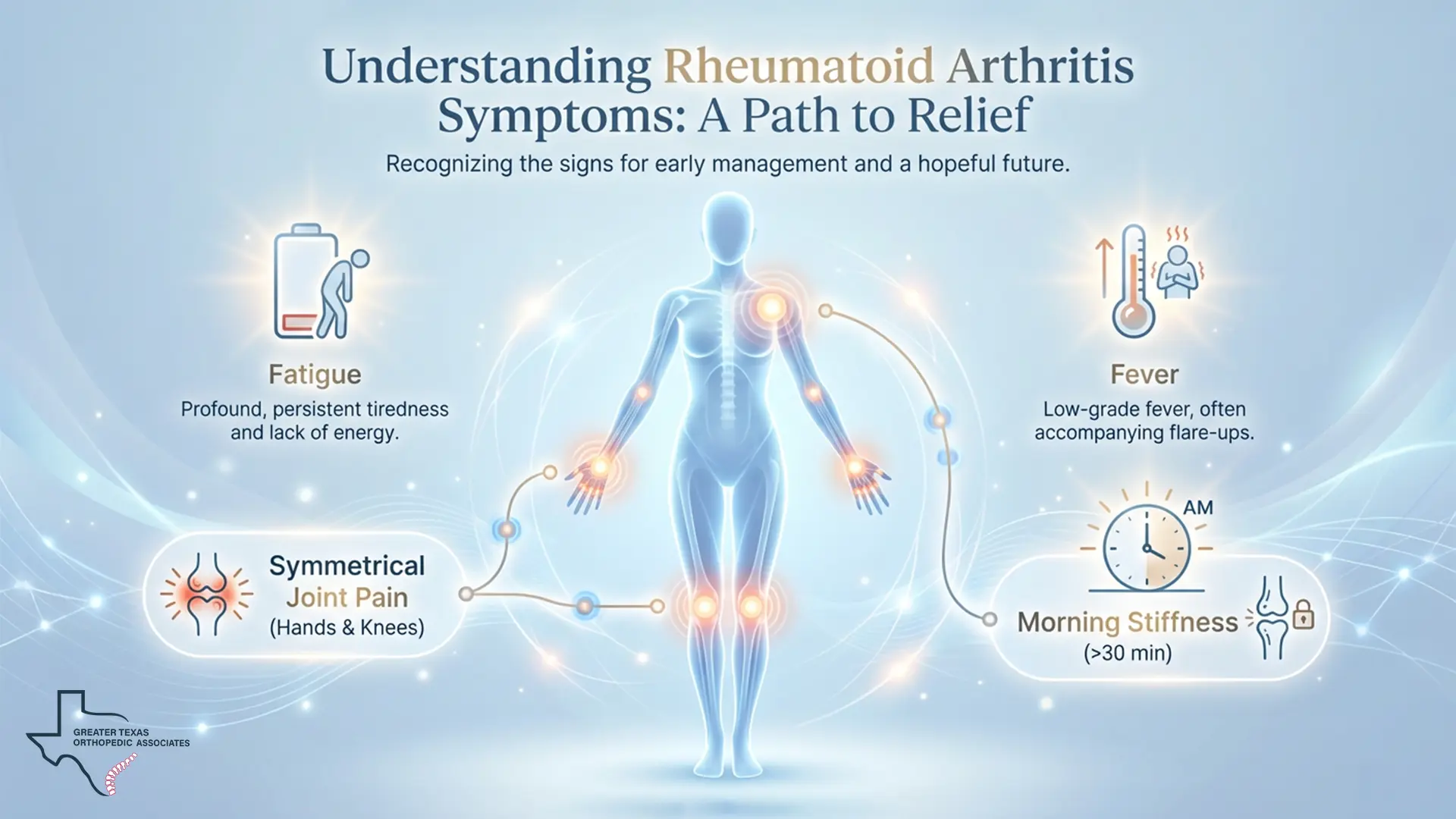
The joint rheumatism symptoms associated with this disease are often symmetric and affect the small joints first, such as those in the fingers, hands, wrists, knees, ankles, feet, and toes. Recognizing these patterns is key to early diagnosis and treatment.
Common joint rheumatism symptoms of this condition include:
- Persistent pain, swelling, stiffness, and tenderness in more than one joint, lasting for six weeks or longer.
- Symmetrical involvement, meaning the same joints are affected on both sides of the body (e.g., both knees or both hands).
- Joint stiffness that is typically worse in the mornings or after periods of rest and can last for 30 minutes, 45 minutes, or even more than one hour before improving with movement. Pain caused by osteoarthritis, by contrast, often improves after activity.
- Systemic symptoms such as fatigue (extreme tiredness), weakness, fever, and loss of appetite. The fatigue can be profound and does not feel normal.
RA is characterized by periods when symptoms are active, known as flares, followed by periods of remission where swelling and pain are reduced or absent.
Beyond the joints, rheumatoid arthritis is a systemic disease that can affect multiple organs due to circulating inflammatory substances. Potential complications affecting other body systems include:
- Skin: The formation of rheumatic lumps called rheumatoid nodules, which usually form around pressure points like the elbows, but can also form in the heart and lungs.
- Eyes and Mouth: Inflammation can lead to dry eyes and mouth, a condition known as secondary Sjögren’s syndrome.
- Lungs and Heart: This disease increases the risk of inflammation and scarring in the lung tissues, which can cause shortness of breath, and raises the risk of heart problems, including inflammation of the sac around the heart and hardened or blocked arteries.
- Nerves and Blood: Swelling in the wrists can compress the nerves, potentially causing Carpal Tunnel Syndrome. Additionally, it can cause a lower-than-normal number of red blood cells (anemia).
Joint rheumatism causes
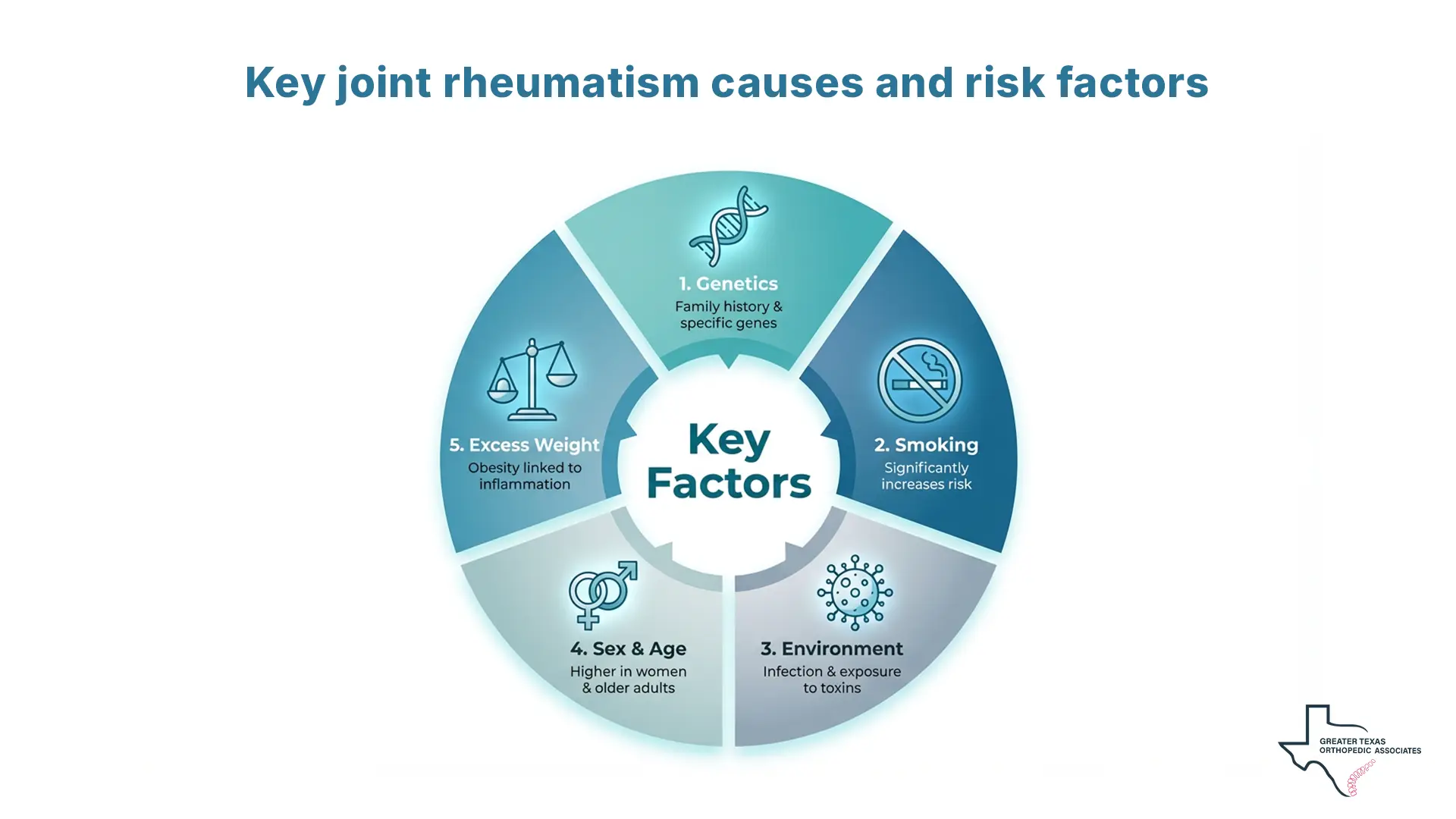
The search for a single, definitive origin for joint rheumatism causes remains ongoing, but experts believe it results from a complex interaction between genetics, hormones, and environmental factors. Essentially, the cause is thought to be a mix of genetic changes and factors from outside the body.
Normally, the immune system acts as a defense mechanism, fighting off invaders. In RA, something triggers the immune system to deregulate and attack the body’s own joint tissue. While no single organism has been conclusively proven to trigger the disease, certain factors are known to increase risk and may activate the immune system in susceptible individuals.
Key joint rheumatism causes and risk factors include:
- Genetic Predisposition: Individuals with variations in specific genes, particularly the human leukocyte antigen (HLA) genes, are more susceptible. A sequence known as the “shared epitope” within these genes is considered the single largest genetic risk factor for the disease.
- Environmental Triggers: External factors, such as certain viral infections, may activate the disease, especially in genetically predisposed individuals.
- Smoking: Cigarette smoking significantly increases the risk of developing the condition and can worsen its severity. This link is particularly strong for those who carry the “shared epitope” gene.
- Gum Infection: Severe gum disease (periodontal disease) is a known risk factor. A specific oral bacterium, Porphyromonas gingivalis, is believed to help trigger the autoimmune response seen in RA.
- Sex and Age: Women are about three times more likely than men to develop the condition. It most commonly begins in middle age, often between 30 and 60 years old.
- Excess Weight: People with obesity have a higher risk, as excess weight puts additional stress on the joints and is associated with persistent back pain.
Rheumatoid Arthritis treatment options
While there is currently no cure for this condition, effective treatment focuses on managing joint inflammation, reducing pain and swelling, maintaining or improving joint function, and preventing long-term joint damage. Early and aggressive treatment is crucial for improving long-term outcomes and slowing disease progression.
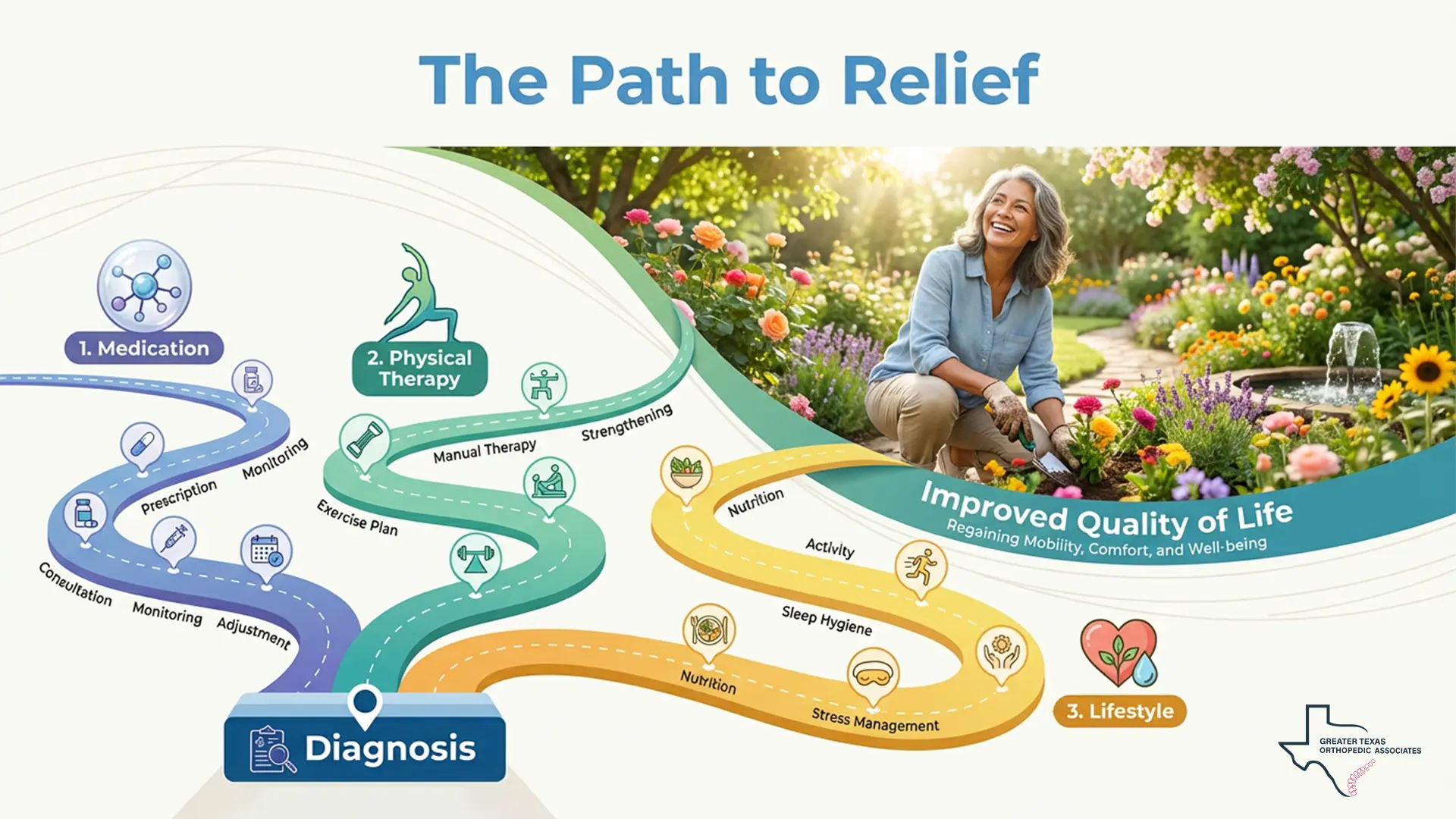
Treatment plans are typically comprehensive and may include a combination of medication, physical therapy, and, in severe cases, surgery.
Medical Management
Medications are the cornerstone of Rheumatoid Arthritis treatment, aiming to reduce pain, control inflammation, and prevent long-term joint damage. Early and combined therapy often leads to the best outcomes.
The main categories of medications include:
Disease-Modifying Antirheumatic Drugs (DMARDs):
Often, the first-line treatment, DMARDs, work broadly to suppress the overactive immune system, slow the progression of the disease, and prevent permanent joint damage. Methotrexate is a widely used example.
Biologics (Targeted Therapies):
When DMARDs are not sufficient, a specialist may prescribe Biologics. These advanced, targeted therapies are designed to block specific inflammatory signals in the immune system. By precisely targeting molecules that cause inflammation (like TNF), they can effectively reduce symptoms and halt joint destruction.
Janus Kinase (JAK) Inhibitors:
These are newer oral medications that work from inside the immune cells. They interrupt the signaling pathways that trigger inflammation, offering another effective way to control the disease, especially when other treatments haven’t worked well.
Corticosteroids (Steroids):
These are powerful, fast-acting anti-inflammatory drugs used for rapid relief during severe flare-ups. They can be taken as pills or injected directly into a joint to quickly reduce pain and swelling, but are typically used for short-term control due to potential side effects.
Interventional Pain Management
For patients experiencing chronic joint pain, whether from RA, osteoarthritis, or facet joint arthropathy, non-surgical pain management techniques can provide targeted, effective relief and often integrate well into a comprehensive Rheumatoid Arthritis treatment plan. These procedures are typically less invasive than surgery and can help reduce pain sufficiently to allow better participation in physical therapy.
At GTOA, we specialize in minimally invasive pain management procedures to address joint and spinal pain. These interventions include:
Facet Joint Injections (FJIs): Delivers a mix of anesthetic and corticosteroid directly into an inflamed facet joint to provide targeted pain relief that can last for several weeks or months.
Medial Branch Blocks (MBBs): A precise diagnostic injection used to confirm if a specific facet joint is the source of a patient’s pain, which helps guide further treatment.
Radiofrequency Ablation (RFA): A long-lasting, minimally invasive solution that uses radiofrequency energy (heat) to disrupt pain signals from a targeted nerve, often providing relief for six months or more.
Epidural Steroid Injections (ESIs): A powerful injection of anti-inflammatory medication into the epidural space to effectively treat pain radiating from inflamed spinal nerves, common in conditions like sciatica. We offer specialized Epidural Steroid Injections services across our Texas locations.
Note: These procedures are aimed at relieving pain and improving function, and are used alongside medical therapy to manage symptoms, not to cure or halt the underlying rheumatoid arthritis.
Rehabilitation and Lifestyle Changes
Physical therapy (PT) is essential in Rheumatoid Arthritis treatment as it helps maintain or increase function, strength, and mobility in affected joints. Exercise can help delay or prevent joint damage.
Recommended lifestyle changes include:
- Physical Activity: Engaging in low-impact aerobic exercises, such as walking, swimming, or cycling, is vital for boosting muscle strength, balance, and fitness, and is often recommended as a first-line intervention for joint pain management.
- Smoking Cessation: Quitting smoking is critically important due to the known association between tobacco use and rheumatoid arthritis progression.
- Diet and Supplements: Maintaining a balanced, nutritious diet is recommended. While no specific anti-inflammatory diet has been scientifically proven to be more effective, supplements like omega-3 fish oil or turmeric may help with pain and morning stiffness, though patients should always consult their doctor first.
- Balancing Activity and Rest: It is important to stay physically active while also incorporating rest, especially during a flare-up, to reduce inflammation and fatigue. Applying heat treatments can soothe stiff joints, while cold treatments are best for reducing swelling and acute pain.
Surgical Intervention
Surgery is generally considered only when medication and other non-surgical treatment options fail to manage pain or when joint damage is so severe that it limits function significantly.
Surgical goals include restoring function to severely damaged joints and correcting deformities caused by long-term inflammation. Procedures may involve:
- Joint Replacement: Replacing severely damaged joints, such as knee replacement, hip replacement, elbow replacement, or shoulder replacement.
- Spinal Surgery: In cases where RA affects the spine (such as the facet joints or causes instability), procedures like spinal fusion may be necessary to stabilize the vertebrae.
Conclusion
Answering what is joint rheumatism means recognizing it as a serious autoimmune condition like rheumatoid arthritis, which requires a proactive and comprehensive treatment plan. The goal is not just to manage symptoms, but to control the underlying disease through a combination of medication, rehabilitation, and effective, non-surgical pain relief procedures.
At GTOA, our focus is on empowering patients on this journey. We provide the specialized evaluations and advanced treatments necessary to create a personalized care plan. By addressing the root cause of your pain and improving function, we help you move beyond the diagnosis of what is joint rheumatism and build a path toward a more active, pain-free life.